Abstract
Background
Management of patients (pts) with primary central nervous system lymphoma (PCNSL) and those with secondary CNS involvement by diffuse large B cell lymphoma (DLBCL) present a therapeutic challenge. There is no clear standard of care but traditionally initial treatment of PCNSL involves induction with intravenous high-dose methotrexate (HD-MTX) followed by consolidation including whole brain radiation therapy (WBRT), cytarabine, or autologous stem cell transplant. This approach has been associated with significant toxicities, especially the risk of cognitive dysfunction with WBRT. Treatment of secondary CNS involvement by DLBCL may depend on the extent of concomitant systemic disease, but HD-MTX is often the backbone of therapy. We report results of our institutional approach in pts with PCNSL and secondary involvement of the CNS by DLBCL using a prolonged course of rituximab, temozolamide, and HD-MTX (RTM) without consolidation.
Methods
We conducted a retrospective cohort study describing outcomes of pts with PCNSL or secondary CNS DLBCL who were treated on the RTM protocol. Eligible pts are treated with rituximab 375 mg/m2 on day 1 in combination with HD-MTX 8 g/m2 (days 1 and 15) and temozolamide 150 mg/m2 (days 1-5) in 28-day cycles. HD-MTX is administered with leucovorin rescue and adjusted for creatinine clearance. Initial response assessment is usually after 2 cycles with brain MRI. Once a complete response (CR) has been achieved, the day 15 HD-MTX is omitted from future cycles. Pts typically complete a total of 6-12 cycles, at the discretion of the clinician, without further planned consolidation.
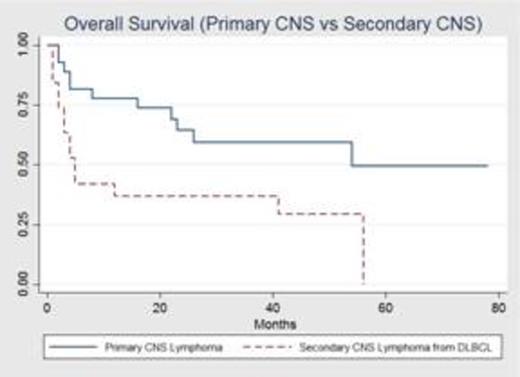
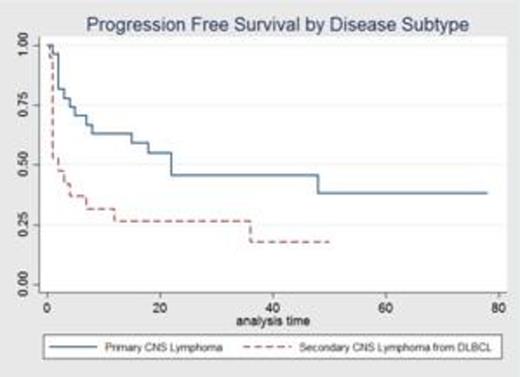
Descriptive and survival analyses using the Kaplan-Meier methodology were performed (STATA 13). The primary endpoints, overall survival (OS) and progression free survival (PFS) were estimated from the date of the first treatment with RTM to death, progression, or date of last follow-up. A log-rank test was utilized to compare OS/PFS between pts with PCNSL versus secondary CNS DLBCL. A Cox proportional hazard analysis was performed to evaluate the effect of patient level variables on OS. Clinical response was evaluated using International Workshop on Response Criteria for PCNSL (Abrey, J Clin Oncol 2005).
Results
We identified 46 pts who received RTM at our institution between 2009 and 2014. Twenty-seven (59%) pts had PCNSL and 19 (41%) pts had secondary CNS DLBCL. The median age at diagnosis was 61 years (range 21-85) with 50% males. Treatment was well tolerated. Two (4%) pts discontinued treatment prematurely and 7 (15%) pts required a dose reduction in HD-MTX due to toxicity. Toxicities included transaminitis, acute renal failure, infection, fatigue, and cytopenias.
In pts with PCNSL, all received RTM as their initial treatment. Best response to therapy in this group was as follows: 19 (70%) had a CR, 3 (11%) had PR, 3 (11%) had SD and 2 (7%) had PD. The overall response rate was 81%. All patients with secondary CNS DLBCL had received prior systemic therapy with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone. Best CNS response to therapy in this group was as follows: 7 (37%) had CR, 2 (11%) had PR, 1 (5%) had SD, and 9 (47%) had PD. The overall response rate was 47%.
For the entire cohort, the median OS was 41 months (m) and median PFS was 8 m. Compared with secondary CNS DLBCL, patients with PCNSL had a significantly longer median OS (54 m vs. 5 m; p<0.01) (Figure 1). PFS was also significantly longer for pts with primary versus secondary CNS DLBCL (22 m vs. 2 m; p=0.02) (Figure 2). Univariate cox analysis demonstrated that sex and age did not impact OS but pts who were in a CR or PR at initial response assessment compared to SD or PD had a hazard ratio for OS of 0.12 (95% CI: 0.05 to 0.29, P<0.01).
Conclusions
In our cohort, pts with PCNSL had excellent outcomes using a prolonged course of the RTM regimen without the toxicities of consolidation with radiation or high dose chemotherapy. These outcomes did not translate to pts with secondary CNS DLBCL, which may be consistent with the different biology and aggressive nature of this subgroup in addition to the prior therapies received. Early response assessment is vital to assess prognosis pts as those who respond within 2 cycles of therapy have an improved OS. This data suggests that RTM without further consolidation is an acceptable alternative regimen for PCNSL. Future prospective studies are needed to validate our findings.
Ganetsky:Onyx: Speakers Bureau. Dwivedy Nasta:Millenium: Research Funding; BMS: Research Funding. Mato:Genentech: Consultancy; Pharmacyclics: Consultancy, Research Funding; Pronai Pharmaceuticals: Research Funding; Celgene Corporation: Consultancy, Research Funding; Gilead: Consultancy, Research Funding; TG Therapeutics: Research Funding; AbbVie: Consultancy, Research Funding; Janssen: Consultancy. Schuster:Gilead: Research Funding; Janssen: Research Funding; Hoffman-LaRoche: Research Funding; Celgene: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; Genentech: Consultancy; Nordic Nanovector: Membership on an entity's Board of Directors or advisory committees; Novartis: Research Funding. Svoboda:Celgene: Research Funding; Seattle Genetics: Research Funding; Immunomedics: Research Funding; Celldex: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.