Abstract

The human organic cation transporter-1 (hOCT-1) is the primary active influx protein for imatinib in BCR-ABL1+ cells. A low functional OCT-1 activity (OA) in peripheral blood mononuclear cells (MNCs) at diagnosis is associated with poorer subsequent molecular response and inferior outcomes in chronic phase chronic myeloid leukaemia (CP-CML) patients. We have previously demonstrated that diclofenac, an antagonist of peroxisome proliferator-activated receptor-γ (PPARγ), can significantly increase OA in BCR-ABL1+ cells. In the current study, we systematically assess the correlation between PPARγ and OA using leukemic cell lines and primary MNCs from untreated de novo CP-CML patients. Given the critical role of PPARγ in cell differentiation and the varying levels of PPARγ expression in different cell types, the present study also explored the relationship between the OA and myeloid-specific markers (CD14, CD15 and CD16) in CP-CML patient MNCs.
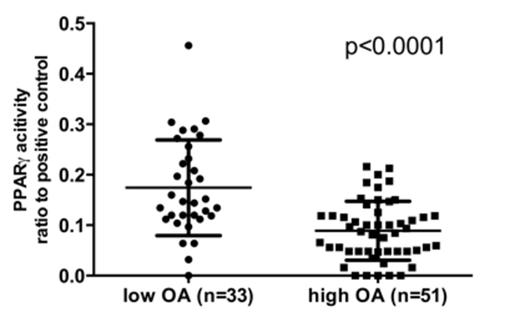
Our results demonstrate that OA in BCR-ABL1 positive and negative leukemic cell lines (KU812, HL60 and HL60-BCRABL1) were significantly decreased with PPARγ agonists (GW1929, rosiglitazone) and increased with antagonists (GW9662, T0070907) (Table 1). Similarly, OA in PPARγ-transduced K562 cells (16.03 ng/200,000 cells) was significantly reduced when compared with empty vector control (22.73 ng/200,000 cells, p=0.028). In primary MNCs isolated from untreated CP-CML patients with high OA, a consistent inhibitory effect on OA was observed following the treatment with PPARγ agonists in all 5 cases. The average OA was significantly reduced by GW1929 (from 7.88 to 5.21 ng/200,000 cells, p=0.0075) or rosiglitazone (to 4.65 ng/200,000 cells, p<0.0001). In contrast, following treatment with PPARγ antagonists, OA was increased in all but one of the low OA patient samples (n=6). The average OA in these patients was increased from 2.71 to 5.07 ng per 200,000 cells by GW9662 (p=0.0129) and to 4.71 ng per 200,000 cells by T0070907 (p=0.0155). In addition, in combination with imatinib, these effects on OA resulted in corresponding changes in Bcr-Abl kinase inhibition and cell viability. While there was no correlation between OA and the expression of the PPARG gene or total PPARγ protein, there was a negative association between OA and PPARγ transcriptional activity in MNCs samples isolated from 84 untreated CP-CML patients (r=-0.5677, p<0.0001, Figure 1). Interestingly, in primary CML samples, the percentage of CD15+ CD14- CD16high MNC cells was significantly higher in patients with low OA (41.70%, n=10) than those with high OA (21.74%, n=11, p=0.0126), which may contribute to the higher PPARγ activity observed in these cases.
In summary, the findings presented in this study highlight for the first time the association between active influx of imatinib and PPARγ. The consistent OA changes in both in BCR-ABL1 positive and negative leukemic cell lines indicate that treatment with PPARγ ligands significantly alter OA via a likely Bcr-Abl independent mechanism. In CP-CML patients at diagnosis, there is a strong negative correlation between OA and PPARγ activity. By up-regulating OA, PPARγ antagonists significantly increased intracellular imatinib and Bcr-Abl kinase inhibition, that subsequently resulted in increased imatinib induced apoptosis. Therefore, reagents repressing PPARγ activity may improve responses for de novo CP-CML patients with low OA. In addition, the CD15+ CD14- CD16high subset of MNCs is significantly enriched in low OA samples providing a potential readily translatable biomarker for a patientÕs molecular response to imatinib.
OCT-1 activity changes in cell lines and MNC from CP-CML patients after treatment with PPARγ ligands (percentage of vehicle control)
| . | PPARγ agonists . | PPARγγ antagonist . | ||
|---|---|---|---|---|
| GW1929 . | Rosiglitazone . | GW9662 . | T0070907 . | |
| KU812 | 67%** | 49%** | 139%** | 151%** |
| HL60 | 75%** | 77%* | 123%* | 123%* |
| HL60-BCRABL1 | 74%* | 79%* | 118%* | 136%** |
| . | PPARγ agonists . | PPARγγ antagonist . | ||
|---|---|---|---|---|
| GW1929 . | Rosiglitazone . | GW9662 . | T0070907 . | |
| KU812 | 67%** | 49%** | 139%** | 151%** |
| HL60 | 75%** | 77%* | 123%* | 123%* |
| HL60-BCRABL1 | 74%* | 79%* | 118%* | 136%** |
*, p<0.05; **, p<0.01; compared with vehicle control.
Levels of PPARγ transcriptional activity were compared between low OA (less than or equal to 4 ng/200,000 cells) and high OA (greater than 4 ng/200,000 cells) groups. The error bars represent 95% confidence interval (CI) of the mean value.
Levels of PPARγ transcriptional activity were compared between low OA (less than or equal to 4 ng/200,000 cells) and high OA (greater than 4 ng/200,000 cells) groups. The error bars represent 95% confidence interval (CI) of the mean value.
Hughes:ARIAD: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. White:Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract