Abstract

BACKGROUND: Ruxolitinib (RUX) is a potent JAK1/JAK2 inhibitor that demonstrated improvements in splenomegaly and disease-related symptoms, as well as improved survival, in patients (pts) with intermediate (Int)-2- or high-risk myelofibrosis (MF), and has proved superior to placebo and best available therapy in the phase 3 COMFORT studies. JUMP is an expanded-access phase 3b trial designed to assess the safety and efficacy of RUX in pts with MF and includes patients with no access to RUX outside a clinical trial. As of Dec 2014, final enrollment was 2233 pts in 26 countries.
METHODS: Eligible pts had Int-2- or high-risk MF with or without splenomegaly, or Int-1-risk MF with a palpable spleen (≥ 5 cm from the costal margin). Pts received starting doses of RUX based on platelet counts at baseline (5 mg twice daily [bid; ≥ 50 to < 100 × 109/L], 15 mg bid [100 to 200 × 109/L], or 20 mg bid [> 200 × 109/L]). The primary endpoint was assessment of safety and tolerability of RUX. Additional analyses included changes in palpable spleen length and symptom scores as measured by the FACT-Lymphoma total score (FACT-Lym TS). The final analysis will be performed after all pts have completed 24 months of treatment or discontinued the study.
RESULTS: This analysis includes 1869 pts (primary MF, 59.1%; n = 1105) who started treatment ≥ 1 year before the data cutoff date (01 Jan 2015). At baseline, median age was 67 y (range, 18-89 y); 54.1% were male; median palpable spleen length was 12 cm below the costal margin; 87 pts did not have splenomegaly. Median hemoglobin (Hb) was 106 g/L, and 38.9% of pts had Hb levels ˂ 100 g/L; median platelet count was 257 × 109/L; mean FACT-Lym TS and FACIT-Fatigue score were 113.7 and 33.2, respectively. At data cutoff, 37.0% of pts remained on treatment; 26.1% had completed treatment per protocol. Primary reasons for discontinuation included adverse events (AEs; 17.4%), disease progression (8.2%), and death (3.4%).
Median exposure was 13.6 months; the median average daily dose was 36.7 mg for pts starting at 20 mg bid (n = 1168; 62.5%) and 23.2 mg for pts starting at 15 mg bid (n = 559; 29.9%). The majority of pts (66.0%) had dose modifications, and 26.2% had a dose interruption.
Grade 3/4 hematologic AEs included anemia (34.0%), thrombocytopenia (14.9%), and neutropenia (3.9%), which led to discontinuation in 2.2%, 3.3%, and 0.2% of pts, respectively. The most common nonhematologic AEs (≥ 10%) were pyrexia (14.5%), asthenia (13.8%), diarrhea (12.4%), and fatigue (10.3%), and were primarily grade 1/2; grade 3/4 AEs were low overall (≤ 2%), except pneumonia (3.9%), which led to discontinuation in 9 pts (0.5%). Rates of infections were low; all-grade infections ≥ 5% included pneumonia (6.2%), urinary tract infection (5.7%), and nasopharyngitis (5.3%). Tuberculosis was reported in 5 pts (0.3%; grade 3/4, 0.1%); hepatitis B was reported in 1 pt (0.1%; grade 3/4, 0.1%).
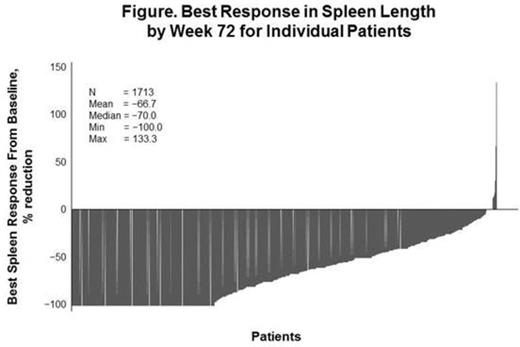
At wk 24 and 48, 57.2% (742/1297) and 62.0% (588/949) of pts with baseline splenomegaly achieved a ≥ 50% reduction from baseline in palpable spleen length; 22.9% (297/1297) and 19.0% (180/949) had 25% to 50% reductions, respectively. Most pts (70.5%; 1208/1713) experienced a ≥ 50% reduction at any time; 23.3% (399/1713) had complete resolution of splenomegaly (Figure). At wk 24 and 48, 96.6% (57/59) and 91.5% (43/47) of evaluable pts without splenomegaly at baseline continued to have a nonpalpable spleen; 1.7% (1/59) and 4.3% (2/47) had a spleen that was 0-5 cm, and 1.7% (1/59) and 4.3% (2/47) had a spleen ≥ 5 cm. A large proportion of pts achieved a response (ie, a clinically significant improvement) on the FACT-Lym TS and FACIT-Fatigue at wk 24 (43.0% [525/1220]; 47.1% [593/1258]) and wk 48 (43.2% [368/852]; 45.7% [396/867]). Similar responses were seen in pts without a palpable spleen (FACT-Lym TS: wk 24, 44.0% [22/50]; wk 48, 36.1% [13/36]; FACIT-Fatigue: wk 24, 49.1% [27/55]; wk 48, 35.1% [13/37]).
CONCLUSIONS: To date, JUMP includes the largest cohort of pts with MF treated with RUX. Consistent with previous findings, anemia and thrombocytopenia were the most common AEs but rarely led to discontinuation. As observed previously, most pts experienced reductions in splenomegaly and symptoms with RUX treatment. Clinically meaningful improvements in symptoms were also seen in pts with no palpable spleen, a pt group not included in the COMFORT studies. Overall, the safety and efficacy profile of RUX in JUMP is consistent with that in the phase 3 COMFORT studies.
Palumbo:Novartis: Honoraria, Other: Advisory Board. Le Coutre:Novartis: Honoraria. Al-Ali:Celgene: Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Ullrich:Novartis: Honoraria. Brittain:Astellas: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pierre Fabre: Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Honoraria, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Foltz:Promedior: Research Funding; Gilead: Research Funding; Novartis: Honoraria, Research Funding. Raanani:Bristol-Myers Squibb: Other: Advisory Board; Novartis: Other: Advisory Board, Research Funding; Ariad: Other: Advisory Board; Pfizer: Other: Advisory Board. Gupta:Incyte: Honoraria, Research Funding; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees. Ghosh:Novartis Pharmaceuticals Corporation: Employment. Tannir:Novartis Pharma AG: Employment. Perez Ronco:Novartis Pharma AG: Employment. Vannucchi:Novartis: Other: Research Funding paid to institution (University of Florence), Research Funding; Shire: Speakers Bureau; Baxalta: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract