Abstract

Background: Gene mutations are common (~90%) in patients with chronic myelomonocytic leukemia (CMML) and involve epigenetic regulators (TET2 ~ 60%, ASXL1 ~40%), spliceosome components (SRSF2 ~40%) and signal pathways (RAS ~30%). Of these, thus far, only ASXL1 mutations have been shown to adversely impact overall survival (OS). In the current study, we used a 27-gene panel assay to identify additional prognostically-relevant mutations in CMML and to also determine if number of mutations carries prognostic relevance.
Methods: 175 patients with WHO-defined CMML were included in the study. All patients had bone marrow (BM) biopsies and cytogenetics performed at diagnosis. Targeted capture assays were carried out on BM DNA specimens obtained at diagnosis for the following genes; TET2, DNMT3A, IDH1, IDH2, ASXL1, EZH2, SUZ12, SRSF2, SF3B1, ZRSR2, U2AF1, PTPN11, Tp53, SH2B3, RUNX1, CBL, NRAS, JAK2, CSF3R, FLT3, KIT, CALR, MPL, NPM1, CEBPA, IKZF, and SETBP1.
Paired-end indexed libraries were prepared from individual patient DNA using the NEBNext Ultra Library prep protocol on the Agilent Bravo liquid handler. Capture libraries were assembled according to Nimblegen standard library protocol. Base-calling was performed using Illumina's RTA version 1.17.21.3. Genesifter software was utilized to analyze targeted sequence data. Specific variants were deemed as mutations if they were associated with a hematological malignancy (as identified by COSMIC database), or if they were not associated with a dbSNP
Results: Among the 175 study patients, 66% were males and median age was 70 years. 146 (83%) patients were subclassified as CMML-1. At a median follow-up of 23 months, 146 (83%) deaths and 25 (14%) leukemic transformations were documented. Median survivals were 24 months for CMML-1 and 16 months for CMML-2 (p=0.38). Mutational frequencies were; TET2 46%, ASXL1 45%, SRSF2 45%, SETBP1 19%, CBL 14%, RUNX1 14%, NRAS 12%, U2AF1 8%, SF3B1 6%, ZRSR2 6%, Tp53 5%, DNMT3A 5%, IDH2 5%, PTPN11 5%, SH2B3 5%, JAK2 4%, NPM1 3%, CSF3R 2%, IDH1 2%, EZH2 1%, SUZ12 1%, KIT 1%, FLT3 1%, CALR 1%. 172 patients (98%) had at least one mutation, 21 (12%) had 2, 24 (14%) had 3, 20 (11%) had 4, 9 (5%) had 5, while one (1%) patient had 6 concurrent mutations. Risk stratification was based on Mayo prognostic model: 25% high, 32% intermediate and 43 % low risk.
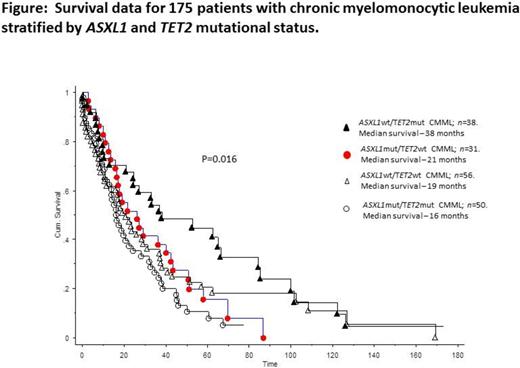
In univariate analysis, presence of ASXL1 mutations (p=0.01), absence of TET2 mutations (p=0.005) and presence of DNMT3A mutations (p=0.02) were associated with inferior survival; in multivariable analysis, ASXL1 (p=0.01) and TET2 (p=0.03) mutations remained significant. In order to determine prognostic interaction between these two mutations, patients were stratified into four mutational categories: ASXL1wt/TET2wt (n =56), ASXL1mut/TET2wt (n =31), ASXL1mut/TET2mut (n =50) and ASXL1wt/TET2mut (n =38). Survival data in these four groups showed significant difference in favor of ASXL1wt/TET2mut (median survival 38 months; p=0.016), compared to those with ASXL1wt/TET2wt (19 months), ASXL1mut/TET2wt (31 months)and ASXL1mut/TET2mut (16 months); there was no significant difference in survival among the latter three groups (p=0.3) (Figure). The number of mutations per patient did not affect outcome (p=0.3).
In multivariable analysis, presence of ASXL1 mutations (P=0.01) and absence of TET2 mutations (p=0.003) remained significant when risk factors used in the Mayo prognostic model (HB <10 gm/dl, AMC >10 x 10(9)/L, platelets <100 x 10(9)/L, circulating IMC) were added to the model; the same was true for ASXL1wt/TET2mut (p=0.036). In a separate multivariable analysis that included the Mayo prognostic model as a single variable along with presence of ASXL1 and absence of TET2 mutations; or absence of ASXL1wt/TET2mut mutational status, the respective hazard ratios were 1.4 (95% CI 1.07-2.1; p=0.012), 1.5 (95% CI 1.07-2.1; p=0.03) and 1.8 (95% CI 1.2-2.7; p=0.001). Leukemia-free survival was worse in ZRSR2 -mutated cases (p=0.03).
Conclusions: Almost 100% of patients with CMML express one or more myeloid neoplasm-relevant mutations. The current study suggests a favorable prognostic impact from TET2 mutations, unless accompanied by ASXL1 mutations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract