Abstract
Aim and Background: Renal impairment (RI) is common feature in patients with multiple myeloma (MM) and is considered as a poor prognostic factor. Improvement of renal function can lead to the improved survival in patients with MM, however little is known on the prognostic impact of reversal of RI compared to that of the patients without RI at diagnosis in the novel agent era. To address this issue, we retrospectively analyzed the impact of RI on survival of newly diagnosed multiple myeloma (NDMM) patients with or without RI seen at our Department over the past 15 years.
Patients and Methods: The study population included all patients diagnosed as MM and treated during May 2000 to March 2015 at Kameda Medical Center, Kamogawa-shi, Japan. We reviewed and retrospectively analyzed the medical records of the Department of Hematology/Oncology. All statistical analyses were performed with EZR, which is a graphical user interface for R ver. 3.2.1.
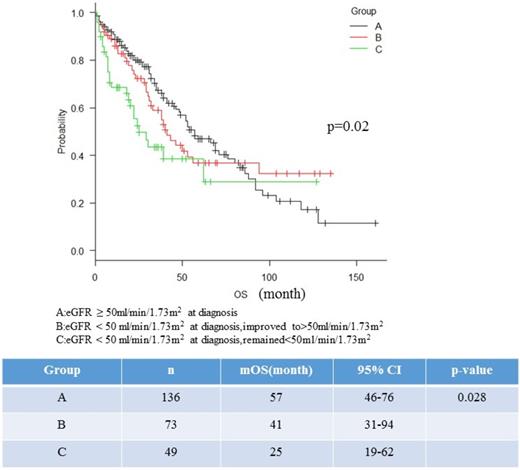
Results: We identified 258 patients with NDMM during this period. RI was defined as eGFR<50ml/min/1.73m2. The median age of patients at diagnosis was 72 years (range 42-90), and 144 patients (55.6%) were male. The median follow-up period for the entire group was 37 months, median serum creatinine at diagnosis was 2.01mg/dL (range 0.4-15) and median eGFR was 52.4ml/min/1.73m2 (range: 2.11-136). RI was observed 122 patients (47.2%). Median serum creatinine of patients with and without RI at diagnosis was 2.07 mg/dL (range: 0.80-4.2) and 0.75mg/mL (range: 0.4-1.1), respectively (p<0.001). Patients with RI had significantly higher proportion of light-chain only disease (39.3% vs 12.5%, p<0.001), International Staging System (ISS) stage 3 (76.2%, vs 31.6%, p=0.001), and lower hemoglobin concentration (Hb<8.5mg/dL: 44.2% vs 21.3%, p<0.001). Bortezomib use, high risk cytogenetics, sex, serum LDH, age at diagnosis, amount of involved immunoglobulin, light chain subtype, and urine albumin at diagnosis were not different between patients with and without RI. Median overall survival (OS) for patients with (n=122) and without (n= 136) RI were 39 months and 57 months, respectively (p=0.16). The median OS for patients with or without RI before and after December 2006, when bortezomib became available in Japan, were 28 months and 41 months (p= 0.66), and 46 months and 71 months (p=0.01), respectively. To evaluate the prognostic impact of renal improvement on survival, patients were divided into 3 groups according to the eGFR and subsequent renal response: Group A; eGFR ≥ 50ml/min/1.73m2 at diagnosis, Group B; eGFR < 50 ml/min/1.73m2 at diagnosis but improved to >50ml/min/1.73m2, Group C; eGFR < 50 ml/min/1.73m2 at diagnosis, and remained <50 ml/min/1.73m2. Median OS of patients with Group A, B, and C was 57 months (n=136), 41 months (n=73), and 25 months (n=49), respectively (p=0.02) (Figure 1). When patients were analysed before and after 2006, the median OS of patients with group A, B, and C before 2006 were 41months (n=59), 38months (n=25) and 19months (n=15) (p=0.02), and those of after 2006 were 71 months (n=77), 46 months (n=48) and not reached (n=34) (p=0.03), respectively. On landmark analysis, median OS at 6 months in each group (Group A, B, and C) were 66 months (n=122), 43 months (n=42), 62 months (n=54), respectively (p= 0.74). Early mortality rate (within 6 months from diagnosis) was significantly higher in patients with group C (16%) compared to other groups (8.5% for group A and 8% for group B, respectively, p=0.03). Patients with group C has significantly higher proportion of mortality rate of infectious disease (26.9%) compared to other groups (7.6% for group A and 11.5% for group B, respectively, p=0.04). Reversal of RI was associated with free light chain (FLC) reduction rate >95% at day 21, age<70years, and treatment response ≥VGPR on univariate analysis, but only FLC reduction rate>95% at day 21 retained its significance on multivariate analysis
Conclusions: Patients with MM with RI showed poor prognosis compared to those without RI. FLC reduction > 95% at day 21 was the independent prognostic predictor for reversal of RI. The higher mortality rate within 6 month of diagnosis observed in patients with RI without renal recovery might attribute to the inferior survival in patients with RI. Although patients with RI with improved renal function had superior survival compared to those without, it remains inferior to the patients without RI at diagnosis
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.