Abstract
Background:
It is estimated that 30-50% of allogeneic hematopoietic stem cell transplants (HSCT) have some type of ABO incompatibility. There are inconsistencies in the literature regarding the impact of recipient/donor ABO mismatch (MM) on HSCT outcomes including overall (OS), event-free survival (EFS), relapse, and acute and chronic graft-versus-host disease (GVHD) in conventional myeloablative or reduced intensity settings. This may be a consequence of heterogeneity in treatment approaches and patient populations studied. In addition, little is known about the effect of ABO MM on outcomes after HI HSCT. To address these issues, we analyzed the effects of various recipient/donor ABO combinations on post HI HSCT outcomes in a population of patients treated on the uniformly designed Jefferson 2-step HSCT method. In this approach, after conditioning, patients received fixed dose of T cells (step 1), followed 2-3 days later by cyclophosphamide (CY) for bidirectional tolerization. Two days after CY, patients received the CD 34-selected donor product (step 2). Our goal was to elucidate the impact of various ABO recipient/donor combinations on outcomes in a homogeneous HI HSCT setting.
Methods:
This is a preliminary, retrospective evaluation of 167 patients with hematologic malignancies undergoing a 2 step HI HSCT between 2006 and 2015. Patients were divided into 3 ABO groups: major MM (MM in recipient to graft direction), minor MM (MM in graft to recipient direction) and matched. The groups were analyzed for the primary statistical end point, the association of ABO incompatible HI HSCT with EFS (death from disease progression or relapse). Secondary end points were the association of ABO incompatibility with OS, non-relapse mortality (NRM) and acute and chronic GVHD. The probabilities of EFS and OS were estimated by Kaplan-Meier (KM) method with log-rank analysis. Multivariate analysis to assess impact of ABO group on EFS and OS controlling for confounding variables (age, disease status at HSCT, conditioning intensity, interval from diagnosis to HSCT) was performed using Cox proportional hazards. Cumulative incidence functions with competing risk analyses were used to estimate probabilities of relapse, NRM, acute and chronic GVHD.
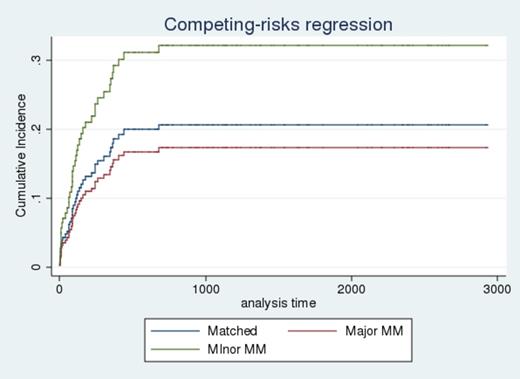
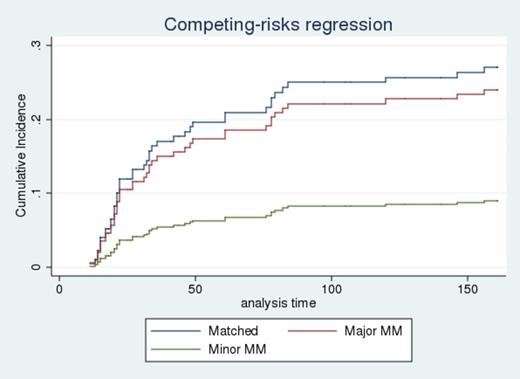
Results: The median age and follow-up of the study group was 55 years and 33.8 months (range: 0.83-97.67 months) respectively. A total of 103 (61.7%) donor-recipient pairs were ABO identical, 28 (16.8%) major MM, and 36 (21.5%) minor MM. KM analysis showed that patients with minor MM had higher EFS but lower OS as compared with matched or major MM groups. This was recapitulated on multivariate Cox analysis, where EFS (HR=0.70, CI 0.30-1.66, p=0.43) was higher, but OS (HR=1.13, CI 0.65-1.97, p= 0.65) was lower in patients with minor MM. On competing risk analysis, NRM was higher (HR=1.67, CI 0.83-3.38, p=0.15) while relapse was lower (HR=0.59, CI 0.27-1.30, p=0.19) in minor MM group. The risk of grades 2 to 4 acute GVHD was significantly lower in patients with minor MM (HR=0.29, CI 0.10-0.88, p=0.02). Risks of acute GVHD grades 3 to 4 and chronic GVHD were not significantly different for any group, possibly due to few events in these categories.
Discussion:
To the best of our knowledge, this is the first assessment of the impact of ABO incompatibility on outcomes after HI HSCT. The strength of this study is the uniformity of treatment protocol and testing group. The analysis suggests that ABO minor MM has different effects on outcomes than major MM or matched groups which were surprisingly similar to each other. These findings were highlighted by the association of minor MM with decreased incidence of acute GVHD, the only finding that reached statistical significance. That minor MM was associated with less relapse and greater EFS may be indicative of a decreased need for immunosuppression in the group, but this relationship does not explain the lower OS and higher NRM in this group. The weakness of the analysis is the small sample size, especially in some subgroups. While most findings failed to reach statistical significance, the analysis was uniform in that minor ABO MM was different from other categories, possibly due to less alloreactivity in this group, thus impacting rates of acute GVHD and survival. These findings support the need for prospective research in this area with larger groups of patients.
Non-relapse Mortality
Acute GVHD 2-4
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.