Abstract
Introduction: Hematopoietic stem cell transplantation (HSCT) requires specialized, resource intensive care. National hospital costs associated with HSCT were $1.3 billion in 2007 (Stranges et al., 2009). Myeloablative conditioning regimens used prior to HSCT tend to be inpatient and more intensive than other preparative regimens, and may therefore be more costly.
Objective: To estimate the total 100-day and one-year costs associated with inpatient HSCT, stratified by type of conditioning regimen and other potential contributors of cost.
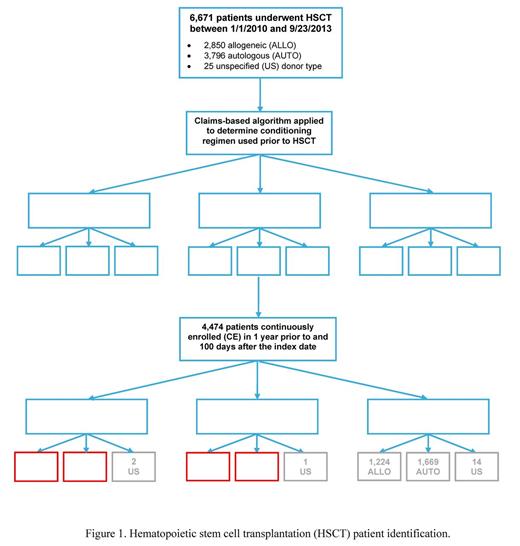
Methods: We used a retrospective cohort study design and MarketScan database to analyze costs among autologous (auto) or allogeneic (allo) inpatient HSCT patients (pts) between 1/2/2010 and 9/23/2013. Because details of chemotherapeutic agents are not available in inpatient claims data, we relied on clinician expert input to develop an algorithm to determine whether conditioning regimens were myeloablative (MA) or nonmyeloablative/reduced intensity (NMA/RIC). The algorithm used the underlying malignancy, type of treatment (e.g. chemotherapy type, radiation), location of service, and therapy timing. Cost estimates in claims are based on amount paid by insurer. Using the date of HSCT as the index date, we examined healthcare use and costs occurring within 100 days and one year of follow-up, according to graft type, conditioning regimen, and age group (pediatric age <18 years).
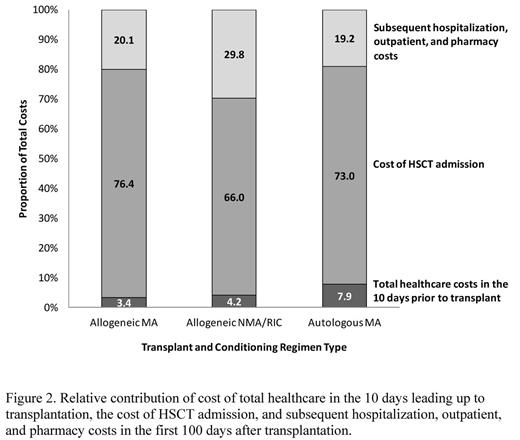
Results: We identified 1,564 pts who had inpatient HSCT for whom graft type and conditioning regimen were determinable (MA allo: n=398; NMA/RIC allo: n=195; MA auto: n=969; NMA/RIC auto: n=2 [Figure 1]). Our sample was 92.9% adult and 61% male. The most common indications for HSCT were lymphoma (62.4%), aplastic anemia (46.3%), acute lymphocytic leukemia (21.5%), and acute myeloid leukemia (11.3%) (not mutually exclusive). In the first 100 days following transplantation, median total healthcare costs were $289,283 for MA allo ps compared to $253,467 for NMA/RIC allo pts and $140,792 for MA auto pts. Mean length of stay (LOS) for the index HSCT hospitalization was 35.6 days for MA allo pts, 26.6 days for NMA/RIC allo pts, and 21.8 days for MA auto pts. Subsequent hospitalization occurred for 42.5% of MA allo pts with a mean LOS of 9 days compared to 43.6% of NMA/RIC allo pts with 11 days and 20.8% of MA auto pts with 6.5 days. Cost of the HSCT admission made up 73-76% of 100-day costs for MA pts and 66% for NMA/RIC pts (Figure 2). 100-day costs were more than two-thirds of total median costs at one year, which were $408,876, $374,065, and $181,933 for the MA allo, NMA/RIC allo, and MA auto group, respectively. Costs for the index HSCT and for 100-day inpatient and outpatient healthcare were greater among pediatric than adult pts, for all graft and conditioning types. Median 100-day pharmacy costs were higher for adults than pediatric pts in the allo but not auto groups.
Conclusions: Total per patient healthcare costs were high in all groups studied, ranging from a median of about $182K to $409K in the one-year period post HSCT.Consistent with prior reports on HSCT, our study comprised predominantly adult, male pts (Majhail et al., 2013; CIBMTR, 2014). Costs varied substantially by graft type, conditioning regimen, and age group, with highest overall 100-day and one-year costs in the MA allo group. Allo HSCT was more expensive at 100 days and one year compared to auto, regardless of regimen. MA conditioning regimen led to higher overall costs compared to NMA/RIC among allo pts, pointing to greater cost burden associated with inpatient services with higher-intensity regimens. Also, pediatric pts had larger 100-day inpatient and outpatient costs compared to adults. These observed differences may have been driven in part by disease severity, malignancy type, body weight, or treatment differences in pediatric and adult pts. Limitations of this initial analysis were that few NMA/RIC auto pts were identified because they are treated in the outpatient setting. In addition, findings were driven largely by the adult pts. Finally, we excluded many pts whose conditioning regimens were undeterminable, making our results sample-specific. Future research should target a broader patient population that includes complete conditioning regimen data and all HSCT regardless of treatment setting.
This analysis was funded by Jazz Pharmaceuticals, Inc.
Quock:Jazz Pharmaceuticals: Employment, Equity Ownership. Broder:Jazz Pharmaceuticals: Other: Partnership for Health Analytic Research (PHAR) received funding from Jazz Pharmaceuticals for study design and analysis; Partnership for Health Analytic Research (PHAR): Employment. Chang:Partnership for Health Analytic Research (PHAR): Employment; Jazz Pharmaceuticals: Other: Partnership for Health Analytic Research (PHAR) received funding from Jazz Pharmaceuticals for study design and analysis. Reddy:Partnership for Health Analytic Research (PHAR): Employment; Jazz Pharmaceuticals: Other: Partnership for Health Analytic Research (PHAR) received funding from Jazz Pharmaceuticals for study design and analysis. Arai:Jazz Pharmaceuticals: Consultancy. Agarwal-Hashmi:Jazz Pharmaceuticals: Consultancy. Villa:Jazz Pharmaceuticals: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.