Abstract
Background: End-of-life (EOL) care has been shown to be more intensive for blood cancers compared to solid tumors (e.g. Hui, Cancer, 2014); however, data are sparse regarding predictors of intensive care unit (ICU) use in the last 30 days of life and hospice enrollment among patients with specific hematologic malignancies. Moreover, little is known about EOL care specifically for the myelodysplastic syndromes (MDS), which are distinguished among the blood cancers by their relative indolence in many patients and high rate of transfusion dependence.
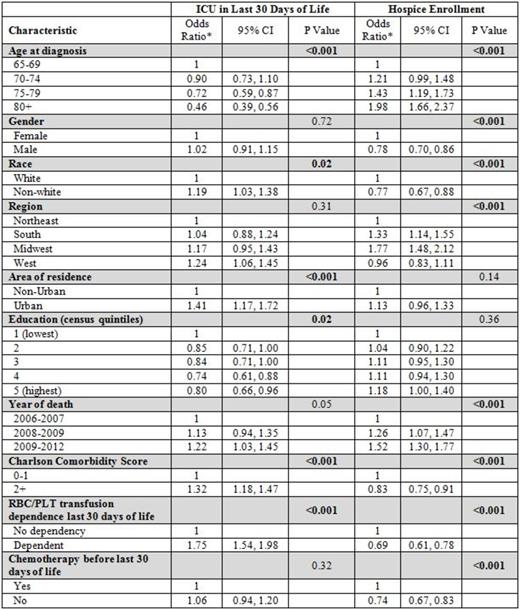
Methods: We conducted a retrospective analysis using the Surveillance Epidemiology and End Results (SEER)-Medicare database. Patients ≥ 65 years of age who had a primary diagnosis of MDS between 2006 and 2011, lived for at least 30 days after their diagnosis, and died prior to December 31, 2012 were eligible for inclusion. Outcomes were two well-established quality measures for EOL care in oncology (Earle, JCO, 2003; Keating, Cancer, 2010): ICU admission within the last 30 days of life (an indicator of poor quality), and enrollment in hospice for any length of time (an indicator of good quality). After determining their overall prevalence, we fit multivariable logistic regression models to investigate sociodemographic and clinical associations (see table) with each outcome.
Results: A total of 6,955 MDS patients were eligible. Overall, 28% were admitted to the ICU in the last month of life, and 49% had enrolled in hospice. In multivariable analyses, transfusion-dependent patients were more likely to be admitted to the ICU and less likely to enroll in hospice (both p<0.001). There was no significant association with marital status or time from diagnosis to death for either outcome. Patients who died in later years had a higher prevalence of ICU admissions (p=0.05) and were more likely to enroll in hospice (p<0.001). Additional multivariable associations are shown below.
*Adjusted for all variables listed as well as marital status and time from diagnosis to death
Conclusions: Only about half of the MDS patients in our cohort were enrolled in hospice; however, the odds of enrollment increased over time. Interestingly, the odds of ICU admission within the last 30 days of life also increased over time, a trend that has been seen in solid tumors (e.g. Wright, JCO, 2014). As bone marrow failure in MDS can lead to reversible sepsis and the need for temporary blood pressure support, it is difficult to determine if this trend truly represents a worsening in quality of EOL care. Finally, our finding that transfusion-dependent MDS patients were less likely to receive hospice suggests that one reason for suboptimal enrollment is that the current hospice model-which largely disallows transfusions-is not meeting the specific palliative needs of this population.
Gore:Celgene: Consultancy, Honoraria, Research Funding. Davidoff:Celgene: Consultancy, Research Funding. Steensma:Incyte: Consultancy; Amgen: Consultancy; Celgene: Consultancy; Onconova: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.