Abstract

Introduction: Thrombotic microangiopathies (TMA) are a group of uncommon disorders characterized clinically by the presence of thrombocytopenia and microangiopathic hemolytic anemia (MAHA). Therapeutic plasma exchange (TPE) is a proven treatment for cases of autoimmune thrombotic thrombocytopenic purpura (TTP) characterized by an ADAMTS13 activity level of ≤10%, but the efficacy of TPE in TMA with an ADAMTS13 activity level of >10% remains controversial.
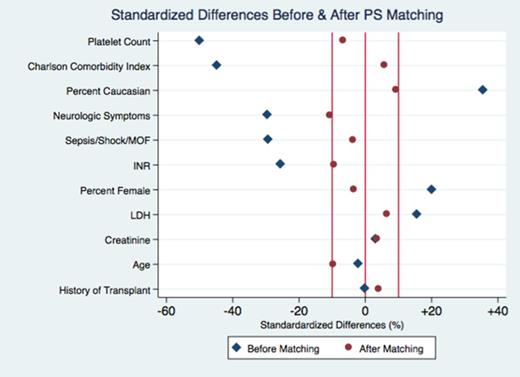
Methods: We conducted a retrospective cohort study of 186 adult patients included in the Harvard TMA Research Collaborative registry who presented with MAHA and thrombocytopenia concerning for TTP but an ADAMTS13 activity level of >10%. A propensity score (PS) logistic regression model was constructed based on 11 clinically relevant confounding variables: age; sex; ethnicity; Charlson Comorbidity Index (CCI); history of prior solid organ or bone marrow transplant; the presence of neurologic symptoms; the presence of sepsis, shock, or multiorgan failure (MOF); platelet count; creatinine; LDH; and INR. Matching was performed using a 1:1 nearest neighbor method without replacement within a set caliper distance. Standardized differences were used to assess the quality of matching and ensure balance of baseline characteristics. The primary outcome was 90-day survival. Secondary outcomes included in-hospital mortality, percent of patients experiencing platelet count recovery, time to platelet count recovery, and hospital length of stay (LOS).
Results: Prior to matching, patients treated with TPE (N=71) had a lower acuity of illness compared to untreated patients (N=115) as reflected by a lower mean CCI (2.3 vs. 3.4, P = 0.003), lower mean INR (1.1 vs. 1.3, P = 0.02), and lower incidence of sepsis, shock or MOF (23% vs. 36%, P = 0.06). Consistent with this confounding, TPE in the pre-matched cohort appeared to be associated with reduced mortality at 90 days (HR 0.51, P = 0.01). The PS match was performed to address these imbalances and resulted in 59 TPE-treated patients paired to 59 untreated controls. After matching, baseline characteristics of the treated and untreated groups were well balanced, with a standardized difference of ≤11% in all PS variables (see Figure).
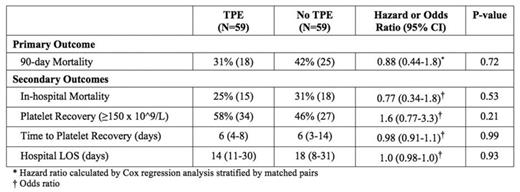
In contrast to the unmatched cohort, Cox regression analysis stratified by matched pairs showed no significant difference in the primary outcome of 90-day survival between the treated and untreated groups (HR 0.88, 95% CI 0.44-1.8, P = 0.72) (see Table). We performed subgroup analyses by age, diagnostic category, and ADAMTS13 activity level and again did not observe any benefit to TPE. With regard to secondary outcomes, in-hospital mortality (OR 0.77, P = 0.53), percent of patients with platelet count recovery (OR 1.6, P = 0.21), median time to platelet count recovery (6 vs. 6 days, P = 0.99), and median hospital LOS (14 vs. 18 days, P = 0.93) did not differ significantly between the two groups.
Conclusions: In the absence of a randomized controlled trial, PS matching represents a rigorous statistical approach to study the effect of treatment while adjusting for differences in baseline characteristics across groups of patients. Here we have used PS matching to assess the efficacy of TPE in the management of TMA associated with an ADAMTS13 activity level of >10%. Our data indicate that there is no benefit from TPE for this diverse group of TMA patients without severe ADAMTS13 deficiency.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract