Abstract

Background: We conducted a phase II study to evaluate the efficacy and safety of dasatinib in patients with newly diagnosed chronic-phase chronic myeloid leukemia (CML-CP) in Japan (IMIDAS PART2 study; UMIN000006358). Several groups reported that some of CML patients who achieved stable deep molecular response (DMR) level or deeper could stop Tyrosine Kinase Inhibitor (TKI) and approximately 40% of these patients could keep therapy free survival by cessation of TKI. Discontinuation of TKI has emerged as a new goal of treatment in CML. Achievement of DMR is necessary for discontinuation of TKI. The aim of the present study was to analyze the prognostic significance of (i) BCR-ABL transcript International Scale (BCR-ABL IS) levels, (ii) the halving time and (iii) velocity of BCR-ABL transcript elimination using an optimized cutoff according to receiver operating characteristic (ROC) analysis.
Methods: Eighty newly diagnosed CML-CP patients were included in this study. Patients received dasatinib 100mg once daily. Treatment has continued until disease progression or unacceptable toxicity. Clinical efficacy and safety was partially reported in 55th ASH Meeting. We sought to investigate the impacts of above 3 parameters within the initial 1 or 3 months of therapy. Halving time was calculated by the method, described by Branford et al. Velocity of BCR-ABL transcript elimination at 1 or 3 months (V-BCR-ABL1m or 3m respectively) was calculated as BCR-ABL IS at 1 or 3 months (BCR-ABL IS1m or 3m respectively) divided by that at diagnosis.
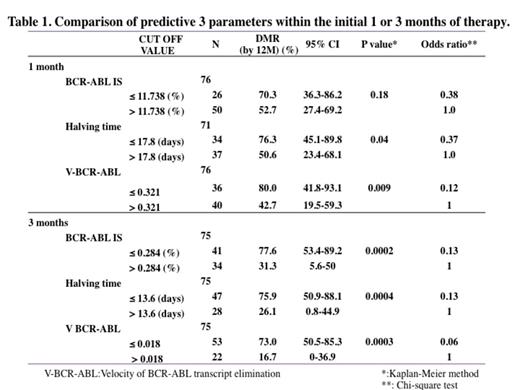
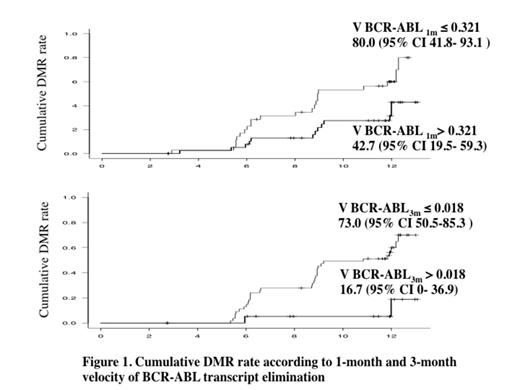
Results: One patient was withdrawal before administration of dasatinib. Seventy-nine patients administered dasatinib 100 mg once daily. The estimated MMR and DMR rates were 92.1 % (95%CI, 76.8-97.3 %) and 60.9% (95%CI; 42.3-73.4 %) by 12 months respectively. The patients who had already achieved DMR at 3 months were excluded from landmark analysis. The cut off values for prediction of DMR at 12 months were obtained by ROC analysis. Those of BCR-ABL IS1m and BCR-ABL IS3m were 11.7% and 0.284% respectively. Those of halving times on 0-1 month and 0-3months (halving time1m and 3m) were 17.8 and 13.6 days respectively. Those of V-BCR-ABL1m and V-BCR-ABL3m were 0.321 and 0.018 respectively. The estimated DMR at 12 months, 95% CI and probability (P), obtained by Kaplan-Myer analysis, were shown in Figure 1. Odd' ratio, obtained by Chi-square test, was shown in Table 1. The patients with less than 0.321 at V-BCR-ABL1m showed the highest DMR at 12 months (80%), the least probability (P=0.009) and the least odd' ratio (0.175). At 3 months, there were similar data in these parameters among BCR-ABL IS3m, halving time3m and V-BCR-ABL3m. Figure 1 showed the cumulative DMR rate according to the cutoff values in V-BCR-ABL1m and V-BCR-ABL3m. V-BCR-ABL1m 0.321 and V-BCR-ABL3m 0.018 separated best.
Conclusion: These data strongly suggested that V-BCR-ABL1m,3m would be a significant landmark to predict DMR at 12 months as well as BCR-ABL IS1m,3m, halving time1m,3m. Among them, less than 0.321 in V-BCR-ABL1m was identified as an optimized predictive cutoff value of DMR at 12 months.
Ishida:Bristol-Myers Squibb: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract