Abstract
Introduction
The discovery of mutations in the calreticulin (CALR) gene in the majority of JAK2 -V617F negative patients with essential thrombocythemia (ET) and primary myelofibrosis (PMF) (Klampfl et al., 2013; Nangalia et al., 2013) has improved the diagnostic accuracy considerably, and most recently distinct clinical and hematological characteristics according to mutational status have been described (Park et al., 2015). The perspective is to personalize and optimize treatment according to the molecular and clinical landscape. This may be achieved by obtaining more information on responses in myeloproliferative neoplasms (MPN) to existing treatment strategies as assessed by the allele burden. Mutations in the CALR gene have proven to play a major role in oncogenic and immunologic processes (Lu, Weng, & Lee, 2015). In this context, it is highly relevant to explore the effectiveness of interferon-alpha2 (IFN) in reducing the CALR -mutated clone. Until now, only one paper has reported a decrease in allele burden in two patients during IFN treatment (Cassinat, Verger, & Kiladijan, 2014). The objective of this report is to expand current knowledge on this important topic by describing the mutant CALR allele burden over time in a larger group of IFN-treated patients.
Method
Clinical data were collected retrospectively from a single institution on all IFN-treated CALR positive MPN patients with sequential determinations of the mutant allele burden. Type 1 and type 2 mutations were initially identified by a previously published fragment analysis (Klampfl et al 2013). We have developed a Taqman qPCR assay for precise determination of the mutant allele burden of type 1 and type 2 mutations. Stored DNA was subsequently analysed to increase follow-up time.
Results
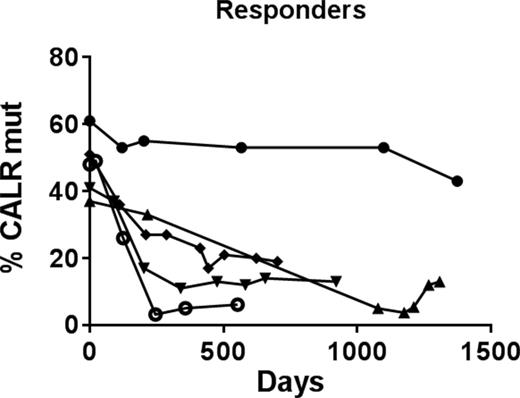
Twenty-one patients were included. Fifteen patients had a diagnosis of PMF; 7 of these were diagnosed with prefibrotic myelofibrosis. Six patients had ET. The type 1 and 2 mutations were found in 15 and 6 patients, respectively. Median age was 60 years (range 42-79) and the sex ratio (M/F) was 8/13. Fifteen patients (71%) were in ongoing treatment with IFN, whereas treatment was discontinued in 6 (29%) because of side effects. Median time of IFN treatment was 756 days (range 42-3927). The IFN prescribed was either subcutaneous injection of Pegasys® (median: 45 microgram (ug) per week), PegIntron® 25-50 ug per week, or Multiferon® 3 x 3 million IU per week. Median follow up time since the first CALR measurement was 756 days (range 294-2108). Fourteen patients (67%) maintained an unchanged allele burden during follow up; 1 patient (5%) presented a temporary decrease (from 39% to 27% in allele burden) but increased to the initial level within months while still on IFN treatment (presumably due to low compliance); 1 patient (5%) displayed an increase in allele burden during transformation to acute myelogenous leukemia (Figure 1); and 5 patients (24%) exhibited a marked decrease in allele burden (median decrease: 32%, range 18-45) during treatment with IFN (Figure 2). All 5 patients with decreasing allele burden (Table 1) normalized their platelet counts within a median time of 5 weeks (range 4-20) after initiating treatment with IFN.
Conclusion
Using a novel sensitive assay for the CALR mutant allele burden, we have demonstrated and substantiated the effectiveness of IFN to reduce the allele burden in a larger series of CALR positive patients with PMF and ET. Importantly, we report for the first time on highly heterogeneous response patterns. Our observation of one fourth of the CALR positive patients responding to treatment with IFN strongly suggests that IFN significantly influences the CALR mutational load. Further clinical and molecular studies are urgently needed to explore the mechanisms behind the heterogeneous response patterns and the clinical implications in regard to clonal evolution and disease progression in non-responding patients. We are currently analysing these issues to assess the definite role of IFN in future treatment strategies in CALR positive MPN patients.
Patients responding to interferon-alpha2
| Characteristics . | Number/median (range) . |
|---|---|
| Patients | 5 |
| Age, years | 53 (42-62) |
| Sex (M/F) | 1/4 |
| Diagnosis - Essential thrombocythemia - Primary myelofibrosis - Prefibrotic myelofibrosis | 2 2 1 |
| Calreticulin mutation type - type 1 - type 2 | 5 0 |
| Duration of interferon-alpha2 treatment, days | 960 (177-2790) |
| Characteristics . | Number/median (range) . |
|---|---|
| Patients | 5 |
| Age, years | 53 (42-62) |
| Sex (M/F) | 1/4 |
| Diagnosis - Essential thrombocythemia - Primary myelofibrosis - Prefibrotic myelofibrosis | 2 2 1 |
| Calreticulin mutation type - type 1 - type 2 | 5 0 |
| Duration of interferon-alpha2 treatment, days | 960 (177-2790) |
Cordua:Janssen-Cilag: Other: travel grant. Off Label Use: interferon alpha2 for myeloproliferative neoplasms. Holmström:La Roche Ltd: Other: travel grant. Pallisgaard:Qiagen: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees, Other: travel grant, Speakers Bureau; Bristol Meyer Squibb: Speakers Bureau; Novartis: Other: travel grant, Research Funding, Speakers Bureau; Roche: Other: travel grant. Hasselbalch:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.