Abstract

Background: Low-molecular weight heparin (LMWH) has been the standard of care for treatment of venous thromboembolism (VTE) in patients with cancer. LMWH injections are painful and costly. Rivaroxaban, an oral direct factor Xa inhibitor, was FDA approved in 2012 for treatment of pulmonary embolism (PE) and deep vein thrombosis (DVT), but there has been a knowledge gap for its use in patients with cancer-associated thrombosis (CAT). Under a Quality Assurance Initiative (QAI), we established a Clinical Pathway to guide rivaroxaban use for CAT, and began to offer rivaroxaban as an alternative to enoxaparin, in January 2014, for patients who met appropriate clinical criteria. We are tracking all cancer patients with PE or symptomatic proximal DVT, whose full course of anticoagulation is with rivaroxaban (allowing up to 3 days of initial parenteral anticoagulation). We now report the characteristics of the first 200 patients, and an outcome analysis of our first 100 patients, who have been treated for at least 6 months or otherwise reached an endpoint.
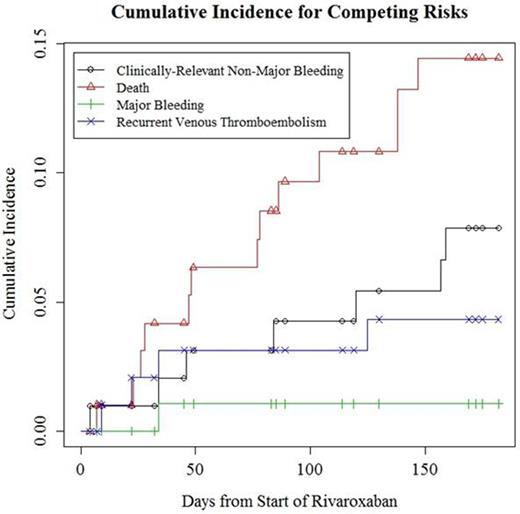
Materials and Methods: The Clinical Pathway guidelines will be available on request, pending publication. Patients were not treated with rivaroxaban if they had active gastrointestinal or genitourinary lesions, or had undergone gastric resection due to anticipated excess bleeding risk or reduced absorption. This excluded under 5% of patients. The Pathway provided dosing guidelines in the setting of thrombocytopenia, advanced age, transient renal, or hepatic dysfunction. Primary endpoints include new or recurrent PE, symptomatic proximal lower extremity DVT, major bleeding (ISTH definition), clinically-relevant non-major bleeding leading to discontinuation of rivaroxaban, or death. Considering those outcomes as competing risks, the cumulative incidence of each event type was calculated using R 3.2.0 for Windows and package "Survival".
Results: The characteristics of our first 200 patients are in Table 1. 70% of the patients had PE. Of the solid tumor patients, 65.6% had metastatic disease. The first 100 patients have completed at least 6 months of rivaroxaban anticoagulation or otherwise reached a primary endpoint. At 6 months, the cumulative incidence of death was 14.4% (95% CI=6.8-21.4%), new or recurrent VTE was 4.3% (95% CI=0.1-8.4%), major bleeding was 1.1% (95% CI=0-3.1%), and clinically relevant non-major bleeding leading to rivaroxaban discontinuation was 7.9% (95% CI=2.1-13.3%).
Conclusions: In the analysis of the first 100 patients entered into our QAI program, the rates of major bleeding, and new or recurrent VTE compare favorably to two published studies of LMWH for treatment of cancer associated thrombosis. In the CLOT study (Lee et al, NEJM, 2003) and the Daltecan study (Francis et al, JTH, 2015), the 6-month rates of new or recurrent VTE were approximately 9%, and the rates of major bleeding were 6% and 9.5% respectively. Our final analysis awaits the completion of 6 months follow-up on 200 patients, to be completed in December 2015. But the rates of major bleeding and recurrent VTE at this point suggest safety and efficacy to be at least non-inferior to LMWH, with the advantage of reduced patient burden, and support the ongoing use of our Clinical Pathway.
Our low rate of major bleeding likely is influenced by the exclusion of patients with active GI or GU lesions, who would be expected to have a high bleeding risk with an oral direct anticoagulant. However, we estimate this excluded less than 5% of cancer patients with VTE. Further, we anticipated reduced drug clearance in the elderly, and used a reduced dose for patients greater than 75 years of age. This appeared to be associated with no loss in efficacy, and helped maintain a low rate of major bleeding.
A randomized trial is the optimal approach to establish non-inferiority or superiority of rivaroxaban to LMWH for cancer associated thrombosis. However, our QAI Clinical Pathway provides guidance and reassurance for rivaroxaban use until a randomized trial is conducted.
Baseline Characteristics of Patients
| Characteristic . | Number of Individuals . | |
|---|---|---|
| Gender | Male | 82 |
| Female | 118 | |
| Event Type | PE, with or without DVT | 140 |
| Proximal, Symptomatic Lower extremity DVT | 60 | |
| Cancer Type | Solid Tumor | 186 |
| Hematologic Malignancy | 14 | |
| Cancer Stage (Of Solid Tumors) | No Evidence of Disease (Post-Cancer Surgery) | 11 (5.9%) |
| 1 | 1 (0.5%) | |
| 2 | 4 (2.2%) | |
| 3 | 16 (8.6%) | |
| 4 | 122 (65.6%) | |
| Unknown | 32 (17.2%) | |
| Characteristic . | Number of Individuals . | |
|---|---|---|
| Gender | Male | 82 |
| Female | 118 | |
| Event Type | PE, with or without DVT | 140 |
| Proximal, Symptomatic Lower extremity DVT | 60 | |
| Cancer Type | Solid Tumor | 186 |
| Hematologic Malignancy | 14 | |
| Cancer Stage (Of Solid Tumors) | No Evidence of Disease (Post-Cancer Surgery) | 11 (5.9%) |
| 1 | 1 (0.5%) | |
| 2 | 4 (2.2%) | |
| 3 | 16 (8.6%) | |
| 4 | 122 (65.6%) | |
| Unknown | 32 (17.2%) | |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract