Abstract
Introduction: A simple test to identify recovery of CMV-specific T cell immunity in the post hematopoietic stem cell transplant (HSCT) period could assist clinicians in managing CMV related complications. The current assays of cell mediated immunity require specialised personnel and equipment, take a long time to perform and are often not available in a routine diagnostic laboratory. We therefore assessed CMV-specific CD8+ T cell immunity using a rapid high throughput Quantiferon-CMV assay to characterise the kinetics of CMV-specific immunity following HSCT.
Methods: An observational multi-centre prospective study of allogeneic HSCT recipients who were at risk of CMV disease was conducted. Study bloods were taken pre-transplant and at 3, 6, 9 and 12 months post-HSCT. CMV-specific immunity was assessed using the Quantiferon-CMV assay which quantifies interferon gamma (IFN-γ) production by ELISA following stimulation with 22 CMV peptides derived from pp65, IE1, IE2, pp50, pp28 and gB, as well as a traditional ELISPOT assay using CMV overlapping peptide pools covering pp65 and IE1. The Quantiferon-CMV assay provides qualitative (reactive, non-reactive, indeterminate) and quantitative results expressed as IFN-γ levels (IU/ml). All participants had CMV surveillance with weekly CMV-PCR until day 100 or beyond in presence of graft versus host disease (GVHD). Participants were either managed with universal routine ganciclovir prophylaxis or CMV monitoring with pre-emptive treatment depending on the treating institution. CMV clinical outcomes were classified as (1) CMV disease with clear tissue involvement, (2) treated CMV reactivation (CMV DNA ³600cp/ml plus antivirals) and (3) spontaneous viral control defined as the resolution of any level of CMV DNA without CMV directed antivirals.
Results: The median age of participants (n=94) was 51 years (IQR 40-56) and the most common indication for transplantation was AML (35%). Sixty-three percent of transplants received myeloablative conditioning, 54% had unrelated donors and 9% were umbilical cord transplants. Seventy-three percent of patients underwent pre-emptive CMV monitoring whilst 27% were on universal prophylaxis. CMV clinical outcomes included CMV disease (n=8), treated CMV reactivation (n=26), spontaneous viral control (n=25) and no detectable CMV DNA (n=31). A further 4 patients had low level viremia (CMV DNA<600copies/ml) treated with antiviral agents. CMV reactivation and CMV disease occurred at a median of 48 and 65 days respectively post HCT. Significant risk factors for CMV disease were donor/recipient CMV serostatus R+/D- (p=0.004), umbilical cord transplant (p=0.003) and acute GVHD (p=0.03).
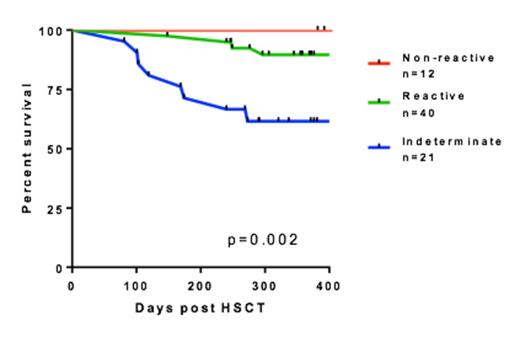
At baseline, there was no difference in the level of IFN-γ producing CMV specific T cells (Quantiferon) between patients who subsequently had CMV disease, CMV reactivation or spontaneous viral control (p=0.24). At 3 months post HSCT patients with CMV disease had significantly lower CMV IFN-γ responses compared to those with CMV reactivation or spontaneous viral control (median IFN-γ 0.04 vs 0.23 vs 1.86 IU/ml respectively, K-Wallis test p=0.001). An indeterminate Quantiferon-CMV result at 3 months was associated with CMV disease (p=0.001) whereas a reactive test was associated with spontaneous viral control (p=0.002). There were no significant differences in CMV IFN-γ levels measured by the Quantiferon-CMV assay results between the clinical groups at 6, 9 or 12 months post HSCT. A significant delay was observed in the time to development of CMV-specific immunity (defined as IFN-γ ³0.1IU/ml) in patients with CMV disease compared to CMV reactivation and spontaneous control (median time 240 vs 110 vs 97 days Mantel-Cox logrank test p=0.02). Twelve month survival was strongly associated with the Quantiferon-CMV result measured 3 months post HSCT being non-reactive, reactive or indeterminate (100% vs 90% vs 61.9% respectively Mantel-Cox Logrank test p=0.002, Graph 1).
Conclusion: At 3 months post HSCT, the results of the Quantiferon-CMV assay which measures CMV-specific CD8+ T cell immunity can identify clinically relevant CMV related outcomes including 12 month survival. The Quantiferon-CMV assay may compliment current CMV prophylactic strategies and assist clinicians to identify patients at high risk of CMV related complications and poor survival.
Twelve month survival curve by 3 month Quantiferon-CMV assay result
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.