Abstract
Background: Standard therapy for intermediate to high-risk acute myeloid leukemia (AML) consists of several hematopoietic cell transplantation (HCT) strategies including autologous-HCT (AUTO), allogeneic-HCT from matched-sibling donor (MSD) or well-matched unrelated donor (WM-URD). When a conventional donor is not available, HCT from partially-matched unrelated donor (PM-URD) or familial mismatched/haploidentical transplantation (FMMT) or umbilical cord blood transplantation is also considered for an alternative choice. Although HCT outcomes of those alternative strategies are advancing with optimization of pre-conditioning regimens with immunosuppressive agents, there are still subjects to debate. We tried to analyze the long-term HCT outcomes according to the donor types including FMMT and PM-URD as an alternative choice.
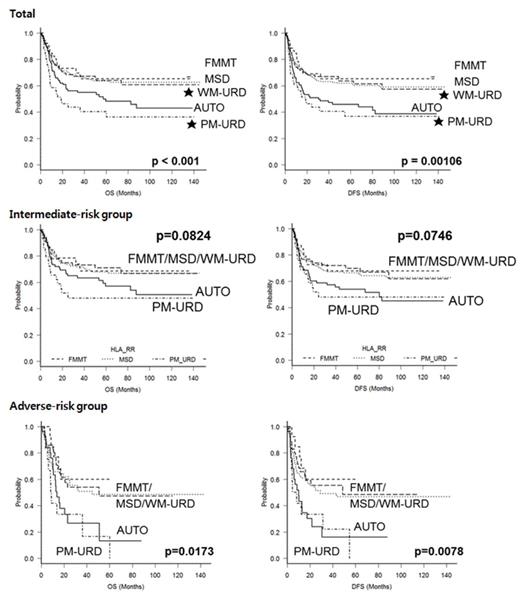
Methods: We enrolled 561 AML patients (median 41 years old, range: 16-68) in complete remission (CR) who were transplanted in Catholic BMT Center in Korea from 2002 to 2013. Patients in at least second CR were excluded. All patients presented intermediate to high-risk karyotype according to the NCCN guidelines, and all of the patients received standard 3+7 chemotherapy followed by consolidation chemotherapy. In the absence of MSD and WM-URD, we allocated PM-URD or AUTO as an alternative choice first, and then FMMT was considered. We divided patients according to the 5 donor types (i.e. MSD (n=252), WM-URD (n=112), PM-URD (n=41), AUTO (n=104), and FMMT (n=52)), and survival outcomes with the cumulative incidence of relapse (CIR), non-relapse mortality (NRM), acute/chronic GVHD and CMV reactivation were analyzed.
Results: Engraftment was successful and showed similar recovery pattern in all donor types. Our data showed mismatch in ABO, sex, and certain HLA locus was not influential, and stem cell source and conditioning-intensity were not also influential for survival outcome and incidence of GVHD. After median follow-up of 54.3 month (range: 6.6-145.6), MSD, WM-URD and FMMT showed similar 5-year OS around 62% except for AUTO at 47.4% and PM-URD at 36.7%. DFS at 5-years was 59% for MSD, 56% for WM-URD, 62% for FMMT, 44.3% for AUTO, and 33.5% for PM-URD. Five-year CIR rate was highest in AUTO (50.3%) followed by PM-URD (33.1%) and WM-URD (29.8%). Lower CIR-rate was identified in MSD (22.4%) and FMMT (21.4%), and the lowest NRM rate was identified in AUTO subgroup (5.1%) followed by WM-URD (11.4%), FMMT (15.6%) and MSD (18.0%). PM-URD showed the highest NRM rate (33.3%) with higher incidence (26.7%) of Gr°Ã3 acute GVHD compared to 9.3% of MSD. Incidence of chronic GVHD was not significantly different. In adverse-risk subgroup, 5-year OS of MSD, WM-URD, and FMMT was 46%, 47%, and 58% respectively, while AUTO and PM-URD was 11% and 0%, which was caused by significantly higher CIR rate of 79.7% and 83.5%, respectively, compared to 31.1% of MSD. In intermediate-risk subgroup, 5-year OS of AUTO (55.2%) was not inferior to that of MSD (67.2%, p =0.330) or FMMT (64.9%, p =0.451), which showed the highest CIR rate (42.8%) and the lowest NRM (5.4%). PM-URD also showed highest NRM (39.4%) with high incidence (27.3%) of Gr°Ã3 acute GVHD.
Conclusions: FMMT should be considered prior to PM-URD in intermediate to adverse-risk AML and GVHD prophylaxis should be intensified when we have to use PM-URD. AUTO might be considered in intermediate-risk AML in selected patients and prospective study should validate the utility of FMMT or AUTO in addition to the conventional donor types.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.