Abstract
Introduction: VOD (also known as Sinusoidal Obstruction Syndrome) is a potentially life threatening complication of hematopoietic stem-cell transplantation (HSCT). Severe VOD (sVOD), defined as VOD with evidence of multi-organ dysfunction (MOD), leads to high morbidity and mortality in HSCT patients. This study assessed healthcare utilization and costs associated with VOD in patients undergoing HSCT.
Methods: A retrospective cohort study was conducted using the Premier research database and had a starting population of all patients with inpatient HSCT between January 1, 2009 and May 31, 2014. The VOD cohort ("all-VOD") included those who also had at least one discharge diagnosis indicating liver injury or at least two diagnoses for VOD symptoms, such as hyperbilirubinemia and/or hepatomegaly, during the study period. sVOD patients were identified using diagnoses for multi-organ dysfunction and were a subset of the VOD cohort. The non-VOD cohort was all patients from the starting cohort who did not have evidence of VOD. Primary outcomes were total hospitalization costs, hospital length of stay (LOS), and inpatient mortality. Secondary outcomes were intensive care unit (ICU) costs, ICU LOS, 30-day all-cause readmission rates and associated costs. Unadjusted descriptive analysis included Chi-squared or Wilcoxon Rank Sum tests for comparisons between cohorts, with non-VOD as the reference group. Multivariable analysis estimated the association between VOD status and primary outcomes, adjusting for differences in demographic, hospital, and clinical characteristics. Generalized linear models (GLM) were applied for total costs and LOS, and logistic regression was used for inpatient mortality. Recycled prediction was used to calculate the adjusted outcomes by VOD status.
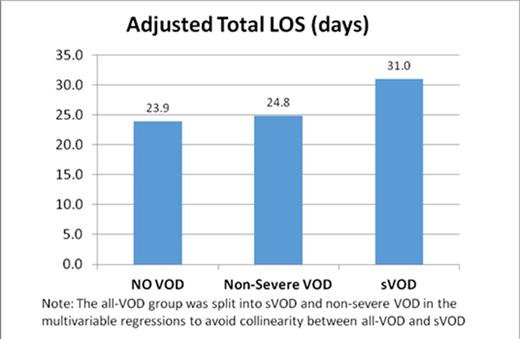
Results: A total of 5,418 patients had inpatient HSCT during the study period. The study included 291 all-VOD patients (134 sVOD and 157 non-severe VOD), in addition to 5,127 patients without evidence of VOD. Unadjusted descriptive analysis found that the all-VOD cohort had higher hospital costs (Median: $119,594, IQR: $59,793-$220,461) and longer LOS (Median: 28 days, IQR: 20-41) than the non-VOD cohort (Median cost: $62,747, IQR: $40,590-$120,974, p<0.001; Median LOS: 21 days, IQR: 16-27; p <0.001). The sVOD sub-cohort had much higher costs and LOS (Median cost: $198,436, IQR: $102,027-$406,683, p<0.001; Median LOS: 37.5 days, IQR: 27-66; p<0.001). Inpatient mortality rates in the all-VOD and sVOD groups were significantly higher than the non-VOD group (non-VOD: 3.0% vs VOD: 18.6%, p<0.001; sVOD: 39.6%, p<0.001). In multivariable regressions, the adjusted hospital costs for non-severe VOD was $8,988 higher than the non-VOD group (p=0.037), and sVOD was $41,703 higher than the non-VOD group (p<0.001). The adjusted hospital LOS for non-severe VOD was 0.90 days longer than the non-VOD group (p=0.023) and for the sVOD group was 7.02 days longer than the non-VOD group (p<0.001). The sVOD group had significantly higher inpatient mortality (10.6%) compared with non-VOD group (3.4%, Adjusted Odds Ratio=5.88, p<0.001), although the mortality difference between non-severe VOD and non-VOD groups was not significant.
Discussion: This analysis is subject to limitations of administrative data. Since there is no diagnostic code for VOD, we used clinical judgment to sort through the codes most likely to be related to VOD/sVOD. Notably, the 40% mortality in the sVOD group is considerably lower than the approximately 80% mortality reported in the literature. One important reason for this difference is that our analysis measured mortality during initial HSCT hospitalization, while the higher rates in the literature are based on 100-day mortality. Additionally, our algorithm may have yielded less severe disease compared to the literature.
Conclusions: VOD and sVOD were associated with increased healthcare utilization and costs compared with the HSCT patients without VOD. sVOD patients also had almost 6 times higher odds of inpatient mortality compared with patients without VOD.
Dvorak:Jazz Pharmaceuticals: Consultancy. Nejadnik:Jazz Pharmaceuticals: Employment, Equity Ownership. Cao:Premier Research Services: Employment; Jazz Pharmaceuticals: Other: Premier Research Services received funding from Jazz Pharmaceuticals for data access, study design, and analysis. Lipkin:Premier Research Services: Employment; Jazz Pharmaceuticals: Other: Premier Research Services received funding from Jazz Pharmaceuticals for data access, study design, and analysis. Robinson:Premier Research Services: Employment; Jazz Pharmaceuticals: Other: Premier Research Services received funding from Jazz Pharmaceuticals for data access, study design, and analysis. Villa:Jazz Pharmaceuticals: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.