Abstract
Introduction:
Venous Thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), is one of the major causes of morbidity and mortality in hospitalized patients. There are limited data regarding the clinical and economic consequences of VTE in patients hospitalized with Non Hodgkin Lymphoma (NHL). The present study aims to assess the impact of VTE on outcomes of hospitalized NHL patients.
Methods:
The study population was derived from the Nationwide Inpatient Sample (NIS) database between the years 2000 and 2012. Using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes, all patients≥18 years of age with NHL were identified. The outcomes were compared between the hospitalized NHL patients with VTE versus those without VTE using the hierarchical multivariate logistic regression analysis. P-value<0.05 was considered statistically significant.
Results:
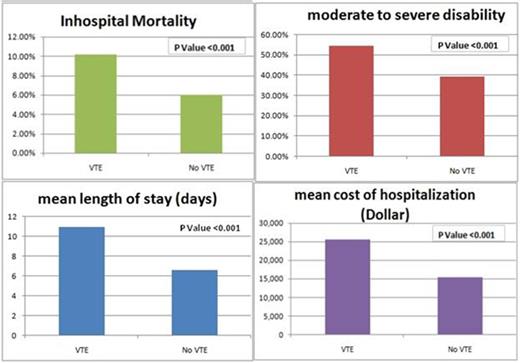
The total number of hospitalizations for NHL patients was 321,857 out of which 15,282 (4.75%) had VTE. The median age of study population was 69 years; 46.58% were females and 79.24% were whites. After adjusting for age, gender, co morbidities and other potential confounders, compared to those without VTE, the NHL patients with VTE had significantly higher rate of in-hospital mortality (10.14% vs. 6.03%, OR=1.72, p<0.01), moderate to severe disability at discharge (54.60% vs. 39.59%, OR=1.85, p<0.01), mean length of stay (10.87 days vs. 6.57 days, OR=1.04, p<0.01), and mean cost of hospitalization ($25,508 vs. $15,307; OR=1.11; p<0.01).
Conclusion:
VTE in hospitalized NHL patients is associated with significant higher inpatient mortality rates, greater disability when discharged and is also associated with longer period of hospitalization and thus increased health care burden. Further studies may be conducted to assess predictor of risk of VTE associated in these complex patients and will help for prevention of VTE and thus decrease the morbidity and mortality and will eventually help decrease health care burden.
Comparison of inpatient mortality, disability, length of stay and cost of hospitalization in Non Hodgkin Lymphoma patients with Venous Thromboembolism as compared to patient without Venous Thromboembolism
| Variable . | Subgroup . | n (total N=321,857) . | Odds Ratio . | LL of 95% CI . | UL of 95% CI . | P-value . |
|---|---|---|---|---|---|---|
| In-hospital mortality | VTE | 14,364 | 1.72 | 1.62 | 1.82 | <0.001 |
| No VTE | 287,768 | |||||
| Moderate to severe disability at discharge | VTE | 14,344 | 1.92 | 1.85 | 1.99 | <0.001 |
| No VTE | 287,513 | |||||
| Length of stay | VTE | 14,375 | 1.04 | 1.038 | 1.041 | <0.001 |
| No VTE | 287,895 | |||||
| Cost ($10,000) | VTE | 13,177 | 1.11 | 1.108 | 1.119 | <0.001 |
| No VTE | 263,697 |
| Variable . | Subgroup . | n (total N=321,857) . | Odds Ratio . | LL of 95% CI . | UL of 95% CI . | P-value . |
|---|---|---|---|---|---|---|
| In-hospital mortality | VTE | 14,364 | 1.72 | 1.62 | 1.82 | <0.001 |
| No VTE | 287,768 | |||||
| Moderate to severe disability at discharge | VTE | 14,344 | 1.92 | 1.85 | 1.99 | <0.001 |
| No VTE | 287,513 | |||||
| Length of stay | VTE | 14,375 | 1.04 | 1.038 | 1.041 | <0.001 |
| No VTE | 287,895 | |||||
| Cost ($10,000) | VTE | 13,177 | 1.11 | 1.108 | 1.119 | <0.001 |
| No VTE | 263,697 |
showing higher inpatient mortality rate, disability, mean length of stay and increased cost of hospitalization in Non Hodgkin Lymphoma patients with Venous Thromboembolism as compared to patient without Venous Thromboembolism
showing higher inpatient mortality rate, disability, mean length of stay and increased cost of hospitalization in Non Hodgkin Lymphoma patients with Venous Thromboembolism as compared to patient without Venous Thromboembolism
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.