Abstract
Background: The heterogeneity of MPN care in Hungary prompted us to establish the Hungarian MPN Working Group (HUMYPRON GROUP) in year 2012.
Aims: The HUMYPRON GROUP created our MPN Registry in 2013, the aims were: (1) to gain epidemiological, diagnostic, therapeutic data, to follow up complications and disease transformations. (2) to investigate the adherence to the WHO/2008 diagnostic criteria and to the Landolfi therapeutic guidelines, to gain insight into vascular and hematological complications (3) to try to identify crucial issues and possible gaps, and promote internationally accepted, standard care in MPN.
Methods: There was close cooperation between hematologists and information technicians (IT) experts to create an easily evaluable questionnaire. Data of classical MPN patients were collected from Hungarian centers. The thrombotic risk and the risk adapted treatment characteristics were stratified according to the Landolfi criteria. The data entry was started in 2014. The centers entered the data of all the essential thrombocythemia (ET), polycythemia vera (PV) and idiopathic myelofibrosis (IMF) patients they had diagnosed and treated.
In the present work we have analysed the tromboembolic (TE) events that have been observed between the diagnosis and data entry, with special emphasis on iron deficiency.
Results: During the first active year of the Hungarian MPN Registry 15 of our major or smaller hematological centers provided patient data, all together reaching the evaluable PV(426)+ET(350) patient number of 776. Because of the method we used entering the data, (all patients of a center) a long follow up period (68 months) was gained, allowing us registering and analyzing 294 TE events. (Table 1)
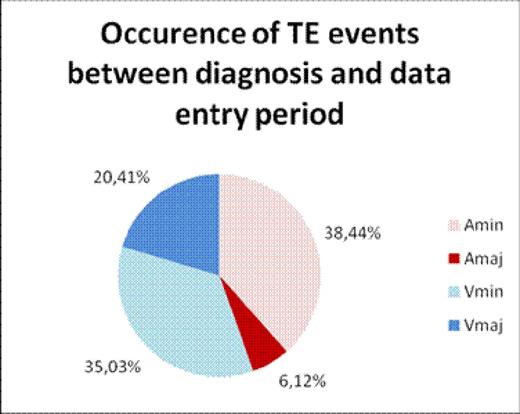
Table 1. Occurence of TE events between diagnosis and data entry period (68 months, 776 PV+ET patients)
Amin: 113 TE events
Amaj: 18 TE events
Vmin: 103 TE events
Vmaj: 60 TE events
Among the 776 PV/ET patients, the data of iron metabolism were registered in 570 records. 142 of them were iron deficient (47 ET/95 PV). There were 73 TE events registered in 142 iron deficient MPN patients and 140 in the iron non deficient (428 patients) group. The male/female ratio, the median age, the median follow up, the Landolfi risk result were similar in the two groups. Comparing the TE events of iron deficient patients to non iron deficients, significantly more events could have been observed in the former group. (Table 2)
Comparison of the TE events in iron deficient /non deficient groups
| TE events . | No of pts . | Male / Female . | Median age (years) . | Follow up (months) . | Landolfi risk result (median) . | Arterial minor . | Arterial major . | Venous minor . | Venous major . | Total TE events . | % of pts having TE . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Iron defficient | 142 | 63/79 | 61,2 | 60 | 4,59 | 31 | 3 | 26 | 13 | 73 | 51% |
| Non defficient | 428 | 193/235 | 60,1 | 62 | 4,53 | 57 | 6 | 51 | 26 | 140 | 32% |
| TE events . | No of pts . | Male / Female . | Median age (years) . | Follow up (months) . | Landolfi risk result (median) . | Arterial minor . | Arterial major . | Venous minor . | Venous major . | Total TE events . | % of pts having TE . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Iron defficient | 142 | 63/79 | 61,2 | 60 | 4,59 | 31 | 3 | 26 | 13 | 73 | 51% |
| Non defficient | 428 | 193/235 | 60,1 | 62 | 4,53 | 57 | 6 | 51 | 26 | 140 | 32% |
The Chi-square statistic is 6.82. The p value is 0.009014. This result is significant at p < 0.05.
Phlebotomy in PV patients and aspirin in both (PV and ET) groups seemed to be worsening the high thrombotic risk caused by iron deficiency, observed at the time of diagnosis, but the result was not significant.
There were 7 major bleeding episodes in the iron deficient group and 12 in the non deficient. Transformation to myelofibrosis occurred in 9 out of 142 patients with iron deficiency and 12 patients in the 428 non iron deficient patients.
The p value is 0.06. This result is significant at p < 0.1.
Conclusions:
1. We have created a national MPN Registry covering a large part of Hungary. The database is operational, online, user friend, easily adjustable to the new professional needs. It is convenient for complex search, correlation and other multiparametric analysis. The data collected so far are in concert with the international epidemiological data.
2. The earlier publications (PVSG) showed iron deficiency as a protective factor in PV patients. Here we report an opposite result, based on the data of a large number of PV+ ET patients and a very long follow up period. When comparing the frequency of the major thrombotic events both group showed the same very low TE frequency, but iron deficiency was found to be significantly inferior when total thrombotic risk and the frequency of minor thrombotic events was evaluated.
3. There were slightly more major bleeding episodes in the iron deficient group.
4. There were significantly more transformation to myelofibrosis in the iron deficient group.
Judit:Semmelweis University First Department of Internal Medicine, Division of Haematology: Employment, Other: advisory board BMS, Roche, Novartis, Amgen.
Author notes
Asterisk with author names denotes non-ASH members.