Abstract
BACKGROUND: The survival expectations of adults with AML have significantly improved over the last 4 decades, partly due to supportive care advancements that have enabled the delivery of increasingly intensive treatment modalities. Even today, however, mortality is high and long-term sequelae are substantial for adults with AML if ICU support becomes necessary. Thus far, information on risk factors for ICU admission and subsequent outcomes in these patients largely stems from small, single-institution studies. Additionally, existing studies have not focused on resource utilization or cost. We therefore utilized the University HealthSystem Consortium (UHC) database to examine risk factors, length of stay (LOS), mortality, and cost associated with ICU admission for adults with AML hospitalized in centers across the United States (U.S.) over a 9-year period.
METHODS: A longitudinal discharge database derived from 239 U.S. UHC participating hospitals was used to retrospectively study adults with AML hospitalized between 2004 and 2012. Clinical data from discharge summaries from each hospital was extracted by certified coders and cost data from all payers was analyzed. This data was then merged to create the central UHC database. To identify the patient population of interest, we developed inclusion criteria based on ICD-9 CM code information. To be included, patient claims had to contain a diagnosis of active AML. Patients were excluded if their disease was in remission or if they had undergone a hematopoietic stem cell transplant. For those with >1 admission during the observation period, one hospitalization was selected randomly for analysis. Primary outcomes included total hospitalization duration, ICU admission and LOS, mortality, and cost (adjusted to 2014 dollars). Independent variables included age, gender, race, year of hospitalization, geographic location, hospital size, comorbidities (e.g. cardiac disease, thrombosis), and types of infectious complications. For binary outcomes, risk categories were compared using unadjusted odds ratios (ORs). Data are presented as means, proportions, or ORs followed by their 95% confidence intervals.
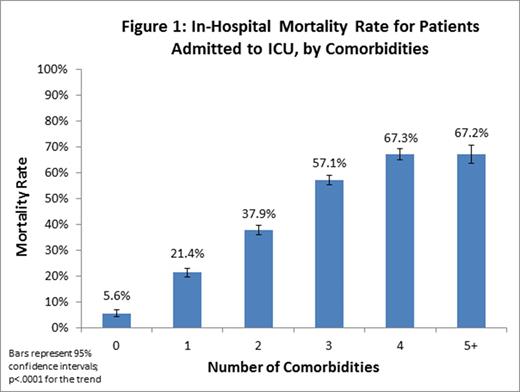
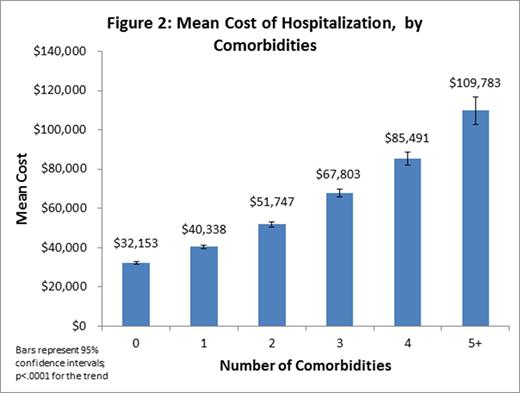
RESULTS: 43,334 hospitalized adult patients with AML were identified. The mean age was 59 years and 41.3% were age ≥65. 54.9% were male, 73.0% Caucasian, 9.6% Black, 4.9% Hispanic, 2.6% Asian, and 9.9% other/unknown. Overall, 26.0% of patients were admitted to the ICU during their hospitalization with a mean ICU LOS of 9.3 days (9.1-9.6). Risk factors for ICU admission included black race (OR=1.2 [1.12-1.29]), hospitalization in the South (OR=1.58 [1.50-1.66]), ≥1 comorbidity (OR=3.61 [3.37-3.86]), and diagnosis of invasive fungal infection (OR=2.35 [2.14-2.59]; p<.0001 for all factors). Overall in-hospital mortality was 17.9% (17.5-18.3%), but was significantly higher for patients requiring ICU care (43.4% vs. 9.0%, p<.0001). Risk factors associated with mortality in those admitted to the ICU included age ≥60 (OR=1.39 [1.29-1.49]), non-white race (OR=1.25 [1.15-1.36]), hospitalization on the West Coast (OR=1.26 [1.14-1.40]), number of comorbidities (trend p<.0001; Figure 1), and invasive fungal infection (OR=1.89 [1.63-2.18]; p<.0001 for all risk factors). In-hospital mortality for ICU patients remained relatively constant over the observation period: 40.6% of patients requiring ICU support died in 2004 vs. 39.9% in 2012 (trend p=.62). Overall, mean LOS was 16 days and total hospitalization cost was $50,176 ($3,263/ day). Mean hospitalization cost increased with each increasing comorbidity from $32,153 to $109,783 per stay for those with 0 vs. ≥5 comorbidities (trend p <.0001; Figure 2). Costs for patients admitted to the ICU were significantly higher than for those who did not require the ICU at $82,350 vs. $38,766, respectively (p<.0001).
CONCLUSION: ICU admission for adults with AML is associated with high mortality and cost that both increase proportionally with the number of comorbidities.Factors associated with ICU admission and mortality in AML patients include both non-modifiable demographic factors (age, race, and geographic location), and medical characteristics (number of comorbidities and underlying infections). These factors may be useful in identifying patients at increased risk for ICU admission early and provide an opportunity for the testing of primary prevention and intervention strategies.
Walter:Amgen, Inc.: Research Funding; Pfizer, Inc.: Consultancy; AstraZeneca, Inc.: Consultancy; Covagen AG: Consultancy; Seattle Genetics, Inc.: Research Funding; Amphivena Therapeutics, Inc.: Consultancy, Research Funding. Lyman:Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.