Abstract
Introduction: Sickle cell disease is associated with frequent hospitalizations and emergency room visits when patients enter vasooclusive crisis. This is associated with lengthy hospitalization that can be time life interrupting for patients, increase hospital cost, and limit bed availability for other patients. Some patients with sickle cell have higher inpatient requirements than others due to the frequency of crisis. Recognizing the issues associated with this, we began scheduling patients for frequent outpatient IV fluids and pain medication to try and prevent ER visits and lengthy hospital stays. We are reporting the experience of three of our patients who have had the most frequent hospitalizations and emergency room visits.
Methods: Patients who had the highest rate of hospitalizations and emergency room visits were offered regular outpatient intravenous and pain medication during the week (up to four times per week) on an as needed basis. Chairs were reserved for these purposes so on demand therapy could be offered without significant delays. The number of ER visits and hospital stays were counted from 12 months before and 12 months after we started offering this. For one of the three patients, data on length of hospital stay could not be accurately determined due to a lengthy hospitalization for infection rather than sickle cell pain crisis, but his emergency room visits were still counted. Basic hospitalization cost for daily hospital charge was also considered, but additional costs such as drug administration, diet, imaging, etc. were not.
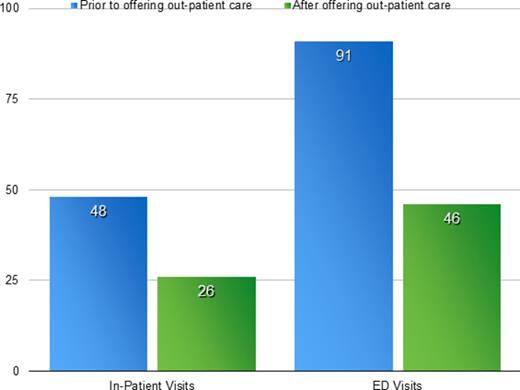
Results: In the 12 months prior to starting regular outpatient IV fluids, there were 48 aggregate emergency room visits compared to 26 in the 12 months after, a reduction of 38%. Inpatient hospital days before were 91 before and 46 post (49%). Cost for hospital days were reduced from $224497 to $113480 (49%).
Conclusion: While offering more outpatient support to our sickle cell patients with the highest hospital demand, we can cut hospital days in half, and limit ER visits and also reduce the cost for inpatient care. Increasing outpatient support, when feasible, should be considered for sickle cell patients who require regular hospitalizations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.