Abstract
Background
With the advancements in relapsed multiple myeloma (RMM) treatments and healthcare resource constraints, it is important to understand the impact of response to RMM treatments on healthcare resource utilization (HRU). We conducted a consensus study in the United States to investigate how HRU may vary by RMM treatment response level.
Methods
A two-round Delphi panel was formed to generate consensus-based estimates of HRU in RMM patients (pts). Ten US hematologists or oncologists meeting the selection criteria (i.e., treated ≥6 RMM pts in the past year; see ≥1 newly diagnosed multiple myeloma pts monthly; spend ≥75% of time in direct pt care) were recruited. All panelists remained anonymous during the process.
In Round 1, each clinician was presented with 16 RMM pt types that varied in age (<65, 65+), ECOG performance status (0-1, 2+), and modified International Myeloma Working Group response levels (complete response [CR], partial response [PR], stable disease [SD], and progressive disease [PD]).
For each pt type presented, physicians were asked to provide annual HRU estimates (in open-ended format) for 11 service categories as informed by pilot telephone interviews with clinicians (e.g., physical exams [PE], emergency room [ER] visits with and without a hospitalization, transfusions, and bone marrow biopsies).
Round 2 focused on categories likely to have a more significant impact on RMM care: PE; ER visits with or without a resulting admission; bone marrow biopsies; supportive prescription medications; transfusions; and PET scans. In this structured survey, a summary of the annual HRU estimates for each pt type and service category from Round 1 was presented. Panelists reviewed blinded, individual estimates obtained in Round 1 and were asked to revisit their own estimates, if appropriate.
Consensus was defined as a priori when ≥75% agreement on categorical items and ≤20% between interquartile range (25th and 75th percentiles) for continuous items. Near consensus was reached when there was 60% to 74% agreement.
Results
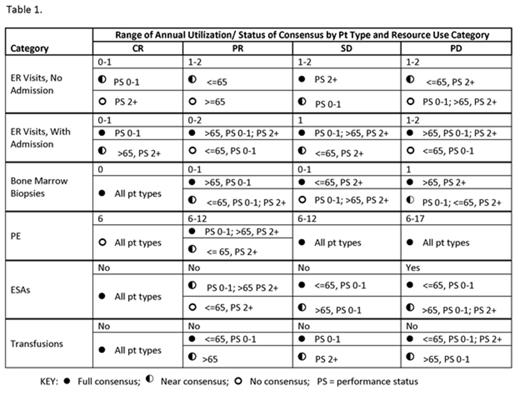
Overall, physicians emphasized the variability of HRU based on pt characteristics and response level. Full consensus was rare, and most often cited in CR. Near consensus was more common, typically in a specific pt type, not by response level (Table 1). However, some generalities can be noted:
For the most costly resources, CR pts are projected to have fewer ER visits (range: 0-1) than non-CR pts irrespective of hospitalization (ER visit with admission: PR 0-2, SD 1, PD 1-2; ER visit, no admission: PR, SD and PD 1-2). Bone marrow biopsy use will likely be higher in non-CR pts (0-1 for PR and SD, 1 in PD vs 0 for CR pts). Non-CR pts are expected to need more PEs (range: 6-17) a year than CR pts (mode: 6). Erythropoietin stimulating agents (ESAs) are unlikely for non-PD pts. Similarly, transfusions are only projected for PD pts.
Consistent with NCCN guidelines, bisphosphonates will be ordered for all pts across response levels. However, antibiotics and G-CSF are likely unnecessary in pts at any response level. The need for PET scans and bone scans/surveys/X-rays could not be adequately determined.
Conclusions
This study demonstrates that CR may be associated with a lower level of resource use in pts with RMM. The importance of novel treatment options for RMM that control the disease more effectively might yield the cost offsets associated with deeper response in those options.
Thomas:Xcenda: Employment. Chen:Onyx Pharmaceuticals: Employment. Bridges:Amgen Inc: Employment. Lankford:Xcenda: Employment. Cong:Onyx Pharmaceuticals: Employment, Equity Ownership. Lee:Xcenda: Employment.
Author notes
Asterisk with author names denotes non-ASH members.