Abstract
Introduction:
Cancer-related fatigue (CrF) is a frequent and disabling symptom in hematological malignancies and associated with significant impairment in quality of life (QoL). Patients suffer from tiredness, weakness and limited capability. CrF involves physical, psychological, mental and social aspects, and often leads to inactivity or depressive mood. There is evidence for the benefit of exercise and physical activity on CrF, but clinical trials targeting patients with MDS are missing.
Methods:
We conducted a prospective, non-randomized trial to assess the feasibility, safety and efficacy of a home-based exercise intervention in patients with IPSS low to intermediate risk MDS. Subjects underwent an introduction and first exercise session at baseline (T0) under supervision of a physiotherapist. Workout sessions were then performed unsupervised in an outpatient setting. Patients were asked to record results in a sports diary. Exercise schedule contained six sessions per week - endurance or strength training in daily turns - over 12 weeks (T1). Follow-up assessment was performed at week 24 (T2).
Endurance training included walking, running, cycling or swimming at patient´s preference. Strength training consisted of six exercises with an elastic strap for both upper and lower limb and the spine. Subjects were examined three times (T0, T1, T2). All examinations included 6-minutes walking distance (6-MWD), an ergometer check, isometric strength measurement of lower limb and isokinetic strength measurement of the abdomen and back. Quality of life and fatigue were assessed by the EORTC QLQ-C30 and Multidimensional Fatigue Inventory (MFI).
Results:
Twenty-one patients (13 male, 8 female) with low to intermediate risk MDS were included. Median age was 66 years (range 29-87). Fifteen patients completed the program at week 12 (T1). Twelve patients voluntarily continued the exercise program until week 24 (T2). The primary endpoint was met, since 11 patients (52%) performed more than 75% of all planned session. Median number of individual workout session was 54 (range 1-72). There were no adverse events reported due to the intervention. Main reasons for missed training sessions were doctor´s appointments or hospitalization, other private appointments, followed by acute infection and general weakness.
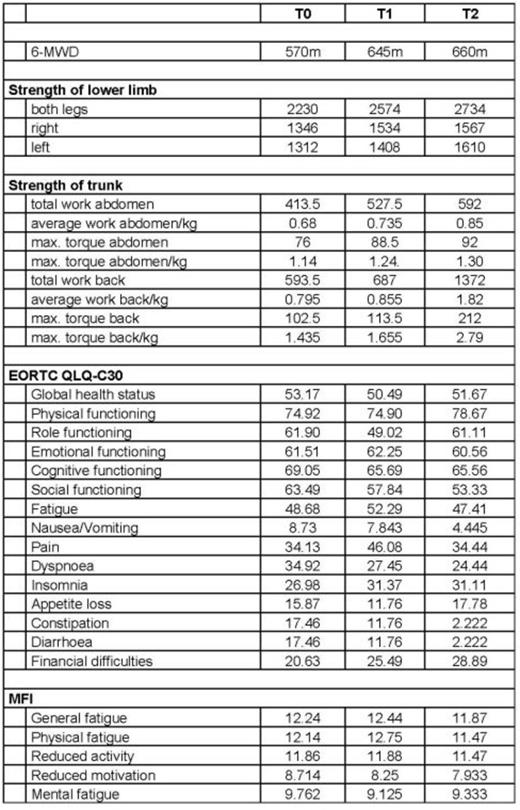
Six-minute walking distance (6-MWD) improved from 570 meters (m) (T0) to 645 m (T1, +13%) and 660 m (T2, +16%). Among other parameters of physical capacity, strength of lower limbs increased from 2230 Newton (N) (T0) to 2570 (T1, +15%) and 2730 (T2, +22%). Between T0, T1 and T2 most functional measures like global health status (53 vs. 50 vs. 52), role functioning (62 vs. 49 vs. 61) and social functioning (63 vs. 58 vs. 53) were equal or slightly decreased. General fatigue did not significantly change over time (49 vs. 52 vs. 47 using the EORTC QLQ-C30 score [scale 0-100] and 12.2 vs. 12.4 vs. 11.9 on MFI [scale 0-21]. Results of all endurance and resistance parameters and QoL measures including fatigue subscales are displayed in Table 1.
Conclusion:
These data provide evidence that an unsupervised outpatient exercise program is feasible in MDS patients. The results of this pilot study also demonstrate that patients' acceptance of the program is high and physical capacity can be improved. Fatigue as a predominant symptom did not worsen during observational period. Further studies are therefore warranted.
Results of all endurance and resistance parameters and QoL measures including fatigue subscales
Results of all endurance and resistance parameters and QoL measures including fatigue subscales
Schuler:PharmaMar: Research Funding. Ehninger:Cellex GmbH: Equity Ownership. Platzbecker:Novartis: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Boehringer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.