Abstract
Introduction
Interim positron-emission tomography (PET) following 1-3 cycles of doxorubicin, bleomycin, vinblastine and dacarbazine (ABVD) in newly-diagnosed, non-bulky stage I and II HL patients (pts) is a useful biomarker that predicts relapse rates of ≤10% for PET- pts. Relapse rates are higher in pts who are PET+ (J Clin Oncol 2014 32: 2705-11; N Engl J Med 2015 372: 1598-607). Interim PET thus provides an opportunity to minimize treatment for the majority of pts who are interim PET - and only intensify treatment for those who are PET+. This strategy could reduce short and long term treatment toxicity for the majority of pts. To test this hypothesis, the US Intergroup conducted a phase II clinical trial, CALGB/Alliance 50604, for newly-diagnosed non-bulky stage I and II HL pts.
Methods
Between 5/15/10 and 5/4/12, 164 previously untreated pts with non-bulky stages I/II HL were enrolled. Pts received 2 cycles of ABVD followed by PET. Deauville scores 1-3 were negative (≤ liver uptake), while scores of 4-5 were positive, based on central review. PET- pts received 2 more cycles of ABVD, and PET+ pts received 2 cycles of dose-intense bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine and prednisone (escalated BEACOPP) + 3060 cGy involved-field radiation therapy (IF RT). Prophylactic growth factor use was permitted only after grade 3/4 febrile neutropenic events, with or without infection.
Results
Median age was 31 years (18-58). There were 88 males and 76 females. Pt. stages were IA (16), IB (4), IIA (90), IIB (35), IIAE 4, and IIBE (3). All pts were PET+ prior to treatment. 144/164 patients had cycle 2 PET and adequate follow-up for assessment: 131 (91%) were PET- and 13 (9%) PET+. Of 20 not analyzed, 13 were excluded (6 never treated and 2 treated with < 2 cycles) and 7 had insufficient follow up.
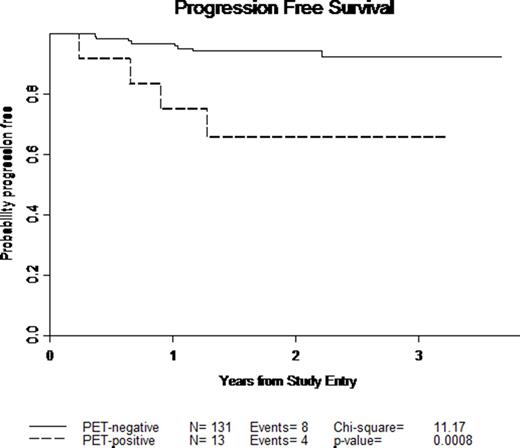
At a median follow-up time of 2 years, 8/131 (6%) PET- pts relapsed or progressed with an estimated 3-year progression-free-survival (PFS) of 92%. 4/13 (31%) PET+ pts. failed (3 relapsed, 1 suicide) with an estimated 3-year PFS of 66%. By Cox model, observed hazard ratio comparing PET- and PET+ PFS for pts is 6.04 (1.82, 20.08). It is likely that the trial will meet the primary objective of 3-year PFS of at least 85% (79%, 92%) for PET- pts treated with 2 additional cycles of ABVD. It is unlikely that the results will meet secondary objective of improving the 3-year PFS of PET+ pts treated with 2 cycles of escalated BEACOPP + IF RT to the pre-set level considered to be of clinical interest in comparison with PET- pts treated with 2 additional cycles of ABVD (HR< 3.84). There was 1 death (suicide).
Toxicity for all pts was minimal: Neutropenia: 29% grade 3 and 42% grade 4; Febrile neutropenia: 5% grade 3; Decreased CO diffusing capacity: 1% grade 3; Decreased left ventricular ejection fraction: 1% grade 3; Sensory neuropathy: 2% grade 3 and 1% grade 4; Motor neuropathy: 1% grade 4.
Conclusions
These early results confirm interim PET as a potential biomarker for prediction of relapse with ABVD in patients with non-bulky, stages I/II HL. Importantly, this study demonstrates that defining PET- as Deauville scores of 1-3 results in only 9% of pts. remaining PET+ after 2 ABVD cycles and excellent PFS for the PET-majority. More intensive treatment with 2 cycles of escalated BEACOPP and IF RT for the 9% of pts who are interim PET+ will be unlikely to improve 3-year PFS to the level considered to be of clinical interest in this trial. Interpretation may be limited by small numbers and lack of randomized control comparison. Fortunately, exciting new treatment approaches may provide an opportunity to improve outcomes for the minority of interim PET+ pts in the future.
Kaplan Meier Plot of PFS for PET-negative and PET-positive patients
For Alliance for Clinical Trials in Oncology, Eastern Cooperative Oncology Group, and Southwest Oncology Group; Supported in part by U10CA180821, U10CA180820, and U10CA180888
Straus:Millenium Pharmaceuticals: Research Funding. Hsi:Abbvie: Research Funding; Cellerent Therapeutics: Research Funding; Eli Lilly: Research Funding; Onyx: Honoraria; Seattle Genetics: Honoraria. Kahl:Roche/Genentech: Consultancy; Seattle Genetics: Consultancy; Millennium: Consultancy; Cell Therapeutics: Consultancy; Celgene: Consultancy; Infinity: Consultancy; Pharmacyclics: Consultancy; Juno: Consultancy. Cheson:Gilead: Consultancy, Research Funding; Teva: Research Funding; Celgene: Consultancy, Research Funding; Ascenta: Research Funding; Astellas: Consultancy; Pharmacyclics: Consultancy, Research Funding; Spectrum: Consultancy; AstraZeneca: Consultancy; Roche/Genentech: Consultancy, Research Funding; MedImmune: Research Funding. Bartlett:Janssen: Research Funding; Pharmacyclics: Research Funding; Astra Zeneca: Research Funding; ImaginAB: Research Funding; Genentech: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Medimmune: Research Funding; Millenium: Research Funding; Celgene: Research Funding; Gilead: Consultancy; Seattle Genetics: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.