Abstract
Background: Multiple myeloma (MM) affects predominantly older individuals but approximately 38% of patients are under the age of 65. Younger patients have benefitted the most from high dose chemotherapy with autologous hematopoietic cell support and subsequently from the introduction of novel agents. While outcomes have improved, care has become more complex and cost-prohibitive, potentially creating barriers to access for disadvantaged patients. The impact of socio economic factors potentially affecting care, namely insurance status, marital status, income and level of education in the outcomes of younger patients with MM is unknown.
Methods: We analyzed MM cases diagnosed in patients < 65 years of age and reported to the Surveillance Epidemiology and End Results (SEER-18) program between 2007 (year when insurance information became available) and 2012 (most recent year available) and characterized the impact of insurance status, marital status, county-level income and county-level education (proportion of adult individuals with bachelor degree) in addition to age, gender, SEER registry and race-ethnicity on survival of MM patients. Risk and corresponding 95% confidence intervals were calculated using multivariable Cox proportional hazard models adjusted for confounders.
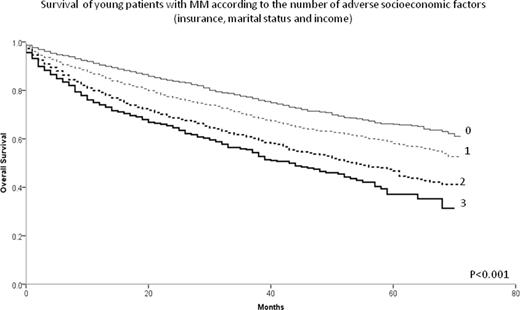
Results: The analysis included 10,161 patients with a median follow up of survivors of 22 months (IQR 8-41 months). Median age at diagnosis was 57 (IQR 51-61), 43.5% were female, 56.2% non-Hispanic Whites (NHW), 24.9% non-Hispanic Blacks (NHB), 13.0% Hispanics, 5.9% of other race-ethnicity category (REC). Uninsured patients comprised 6%, Medicaid beneficiary 14.7%, and 79.3% had insurance benefits other than Medicaid. Married patients were 62.9%, 20.7% were single, 12.9% divorced or separated and 3.5% widowed. As shown in Table 1, increased risk of death was associated with older age, male gender, residence in the area of certain SEER-18 registries, low county-level income, marital status other than married, being uninsured or being Medicaid beneficiary (Table 1). The presence of increasing number of the 3 following independent socioeconomic risk factors: county-level income in the lower two quartiles, not married and being uninsured or Medicaid beneficiary, was associated with incremental worsening in survival (Figure 1). Patients with 0, 1, 2 and 3 socioeconomic risk factors had four year estimated survival of 71.1% (95% C.I. 68.9-73.3%), 63.2% (95% C.I. 61.2-65.1%) , 53.4% (95% C.I. 50.7-56.1) and 46.5% (95% C.I. 41.6-51.4%) respectively (P<0.001). Of interest, while NHB and Hispanics had worse survival in univariate analysis, REC did not contribute to the multivariate survival model.
Conclusions: Insurance status, marital status and county-level income, but not REC and county-level education have a strong influence on the survival of younger patients with MM after adjustment for SEER registry, age and sex. Advances in MM treatment and outcomes disproportionally benefit patients of different socioeconomic backgrounds.
| . | . | Multivariate Analysis . | ||
|---|---|---|---|---|
| Reference | HR | 95% CI | P | |
| SEER registry | 0.001 | |||
| Alaska | Greater California | 0.58 | 0.14-2.33 | 0.4 |
| Atlanta | Greater California | 0.97 | 0.80-1.17 | 0.8 |
| Connecticut | Greater California | 0.81 | 0.65-1.00 | 0.05 |
| Detroit | Greater California | 0.99 | 0.84-1.18 | 0.9 |
| Greater Georgia | Greater California | 0.85 | 0.72-0.99 | 0.04 |
| Hawaii | Greater California | 1.53 | 1.14-2.05 | 0.005 |
| Iowa | Greater California | 1.14 | 0.92-1.41 | 0.2 |
| Kentucky | Greater California | 1.01 | 0.84-1.22 | 0.9 |
| Los Angeles | Greater California | 0.85 | 0.73-0.99 | 0.04 |
| Louisiana | Greater California | 0.96 | 0.80-1.15 | 0.9 |
| New Jersey | Greater California | 0.86 | 0.74-1.00 | 0.05 |
| New Mexico | Greater California | 0.98 | 0.73-1.31 | 0.9 |
| Rural Georgia | Greater California | 2.06 | 1.15-3.67 | 0.01 |
| San Francisco-Oakland | Greater California | 0.90 | 0.73-1.11 | 0.3 |
| San Jose-Monterey | Greater California | 0.89 | 0.68-1.18 | 0.4 |
| Seattle | Greater California | 1.04 | 0.86-1.26 | 0.7 |
| Utah | Greater California | 1.18 | 0.90-1.54 | 0.2 |
| Age | Per year | 1.03 | 1.02-1.04 | <0.001 |
| Female | Male | 0.85 | 0.78-0.91 | <0.001 |
| Marital status | <0.001 | |||
| Divorced | Married | 1.24 | 1.11-1.39 | <0.001 |
| Single | Married | 1.39 | 1.27-1.53 | <0.001 |
| Widow | Married | 1.43 | 1.20-1.71 | <0.001 |
| Insurance status | <0.001 | |||
| Medicaid | Insured | 1.76 | 1.59-1.94 | <0.001 |
| Uninsured | Insured | 1.43 | 1.23-1.67 | <0.001 |
| County-level income | <0.001 | |||
| Quartile 1 | Quartile 4 | 1.27 | 1.09-1.49 | 0.002 |
| Quartile 2 | Quartile 4 | 1.19 | 1.03-1.37 | 0.02 |
| Quartile 3 | Quartile 4 | 0.97 | 0.85-1.10 | 0.6 |
| . | . | Multivariate Analysis . | ||
|---|---|---|---|---|
| Reference | HR | 95% CI | P | |
| SEER registry | 0.001 | |||
| Alaska | Greater California | 0.58 | 0.14-2.33 | 0.4 |
| Atlanta | Greater California | 0.97 | 0.80-1.17 | 0.8 |
| Connecticut | Greater California | 0.81 | 0.65-1.00 | 0.05 |
| Detroit | Greater California | 0.99 | 0.84-1.18 | 0.9 |
| Greater Georgia | Greater California | 0.85 | 0.72-0.99 | 0.04 |
| Hawaii | Greater California | 1.53 | 1.14-2.05 | 0.005 |
| Iowa | Greater California | 1.14 | 0.92-1.41 | 0.2 |
| Kentucky | Greater California | 1.01 | 0.84-1.22 | 0.9 |
| Los Angeles | Greater California | 0.85 | 0.73-0.99 | 0.04 |
| Louisiana | Greater California | 0.96 | 0.80-1.15 | 0.9 |
| New Jersey | Greater California | 0.86 | 0.74-1.00 | 0.05 |
| New Mexico | Greater California | 0.98 | 0.73-1.31 | 0.9 |
| Rural Georgia | Greater California | 2.06 | 1.15-3.67 | 0.01 |
| San Francisco-Oakland | Greater California | 0.90 | 0.73-1.11 | 0.3 |
| San Jose-Monterey | Greater California | 0.89 | 0.68-1.18 | 0.4 |
| Seattle | Greater California | 1.04 | 0.86-1.26 | 0.7 |
| Utah | Greater California | 1.18 | 0.90-1.54 | 0.2 |
| Age | Per year | 1.03 | 1.02-1.04 | <0.001 |
| Female | Male | 0.85 | 0.78-0.91 | <0.001 |
| Marital status | <0.001 | |||
| Divorced | Married | 1.24 | 1.11-1.39 | <0.001 |
| Single | Married | 1.39 | 1.27-1.53 | <0.001 |
| Widow | Married | 1.43 | 1.20-1.71 | <0.001 |
| Insurance status | <0.001 | |||
| Medicaid | Insured | 1.76 | 1.59-1.94 | <0.001 |
| Uninsured | Insured | 1.43 | 1.23-1.67 | <0.001 |
| County-level income | <0.001 | |||
| Quartile 1 | Quartile 4 | 1.27 | 1.09-1.49 | 0.002 |
| Quartile 2 | Quartile 4 | 1.19 | 1.03-1.37 | 0.02 |
| Quartile 3 | Quartile 4 | 0.97 | 0.85-1.10 | 0.6 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.