Abstract
Background:
Transfusion of stored red blood cells (RBCs) results in a variable amount of extravascular hemolysis depending on the extent of RBC damage during storage. Metabolomic studies of RBCs throughout storage in vitro suggest that a shift in the metabolomics profile occurs at 14-21 days of storage; however, the correlation between storage duration in vitro and the extent of hemolysis in vivo is unknown.
Aims:
This study examined the relationship between storage duration and laboratory evidence of hemolysis in human recipients after autologous RBC transfusion.
Methods:
We recruited 30 healthy adults who met the standards for allogeneic blood donation. Each volunteer was randomized to receive a transfusion of one autologous RBC unit after 1, 2, 3, 4, 5, or 6 weeks of storage. Each RBC unit was transfused over 1 hour and blood samples were collected before, and at 0, 2, 4, 8, 10, 12, 14, and 20 hours after transfusion to measure various analytes. Serum hepcidin was measured by ELISA, plasma free hemoglobin by the cyanomethemoglobin method, and all other parameters by standard clinical laboratory assays. For each analyte, the Pearson correlation coefficient was used to determine the strength of the linear association between storage duration and changes in analyte levels at specific times post-transfusion.
Results:
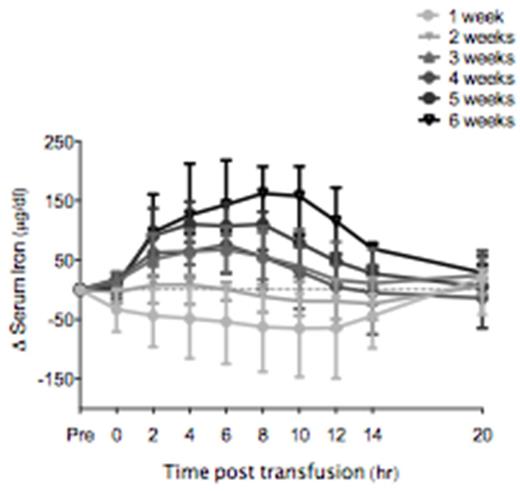
At each time evaluated between 0 and 8 hours after transfusion, indirect bilirubin, a marker of extravascular hemolysis, progressively and linearly increased proportionally with RBC storage duration, with the maximal regression coefficient observed 2 hours post-transfusion (R2 = 0.44; p<0.0001). Furthermore, at all times evaluated between 0 and 14 hours post-transfusion, serum iron increased proportionally with storage duration (see Figure); the strongest regression coefficient was observed 6 and 8 hours post-transfusion (R2 = 0.67; p<0.0001). In conjunction with the increases in serum iron, hepcidin, the master regulator of iron homeostasis, increased proportionally with storage duration at all times between 6 and 12 hours post-transfusion with a maximal regression coefficient at 8 hours post-transfusion (R2 = 0.25; p<0.007). In contrast, no linear associations were found between RBC storage duration and indicators of intravascular hemolysis, including plasma free hemoglobin, lactate dehydrogenase, and haptoglobin.
Conclusion:
Altogether, these results suggest that, as storage duration increases, there is a progressive increase in post-transfusion extravascular hemolysis. Furthermore, this is the first report of an effect of stored RBC transfusions on serum hepcidin concentrations. In particular, progressive increases in hepcidin levels, associated with increased storage duration, are observed starting at 6 hours post-transfusion. Nonetheless, the strengths of correlation coefficients between markers of extravascular hemolysis and RBC storage duration suggest that substantial donor/recipient variability exists. The clinical consequences of the progressive increase in extravascular hemolysis with greater durations of RBC storage remain to be determined.
Median with interquartile range for changes in serum iron levels from baseline (i.e., pre-transfusion) to 20 hours post-transfusion for each randomized week of RBC storage (N=30). Serum iron increased between 0 and 14 hours post-transfusion, with a maximum peak at 6-8 hours post-transfusion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.