Abstract
INTRODUCTION: Sickle cell disease is an inherited blood disorder characterized by vaso-occlusive crises (VOC). HbS in red blood cells (RBC) polymerizes rapidly after it releases oxygen to tissues, causing RBC to become rigid. Anything that decreases flow in the microvasculature increases the chance that this flexible-to-rigid transformation occurs causing the rigid blood cell to lodge in the microvasculature, therefore increasing the chance of vaso-occlusion and the risk of VOC. Although hypoxia and stress are known risk factors for crises, the exact mechanism that initiates VOC events is not well known. We have previously shown that transient hypoxia causes parasympathetic withdrawal and sighs cause vasoconstriction more frequently in SCD subjects than in normal controls. Pain is the hallmark of SCD and is a consequence of VOC but has not been considered as a possible trigger of vasoconstriction that may lead to VOC.
OBJECTIVES: To determine if heat induced pain causes decrease in peripheral blood flow (PBF) in SCD.
METHODS: 30 SCD and 30 control subjects (healthy and sickle cell traits) were recruited at Children's Hospital Los Angeles (CHLA). Quasi-periodic pulses of pain were induced on the right forearm using TSA-II neuro analyzer heating thermode.
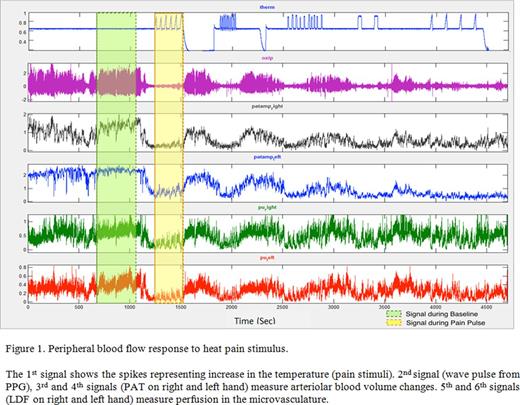
We implemented a technique using cross correlation analysis to detect changes in complex microvascular flow signals measured bilaterally on the hands, using laser-Doppler flowmeter (LDF), Peripheral Arterial Tonometer (PAT) and photo-plethysmography (PPG).
We also measured the average drop from baseline in the microvascular flow during the heat pain. Data were analyzed using one- and two- sample Student t-test.
RESULTS: Data on 53 subjects were analyzed. There was a significant correlation between heat pain pulses and PBF responses, as well as a significant drop in blood flow in all study participants (PPG signal, both p<0.001), indicating that heat pain pulses lead to vasoconstriction.
Males had higher correlation (p<0.005) and stronger vasoconstriction (p<0.05) during heat stimuli compared to females. Other Signals (LDF and PAT) had a similar pattern but were less significant.
The vasoconstriction response consisted of two components, the first one occurred prior to administration of the painful stimulus indicating that anxiety or anticipation of pain causes significant vasoconstriction. Application of the painful stimulus causes further vasoconstriction.
CONCLUSIONS: The findings demonstrate a significant decrease in PBF in both SCD and controls in response to heat pain and possibly to pain anticipation. The decrease in PBF could play a critical role in the genesis of VOC in SCD by markedly prolonging microvascular transit time, increasing the likelihood of red cell entrapment when sickle red cells transform from flexible to rigid. Furthermore, the potent vasoconstriction response to pain in SCD means that pain resulting from VOC could potentially trigger a cascade effect in which vasoconstriction could lead to even more serious VOC. Since regional blood flow is regulated by the autonomic nervous system (ANS), which has been described to be dysfunctional in SCD, our study calls attention to the ANS as a factor in the genesis of crisis in this disorder.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.