Introduction:
Patients with active malignancy who develop venous thromboembolism (VTE) have historically been anticoagulated with a vitamin K antagonist (VKA) such as warfarin. The CLOT study (Lee et al., NEJM, 2003) demonstrated that injection with the low-molecular weight heparin (LMWH) dalteparin was better than warfarin at preventing recurrence of VTE in cancer patients, which changed clinical practice in the United States; however, a subsequent competing risks analysis (Parpia et al., Contemp Clin Trials, 2011) suggested the magnitude of this benefit may be less than previously believed. Neither patient-focused measures of utility nor the cost of each strategy have been evaluated in the current treatment era. We aimed to characterize the effectiveness and costs associated with these two management strategies for malignancy-associated VTE.
Methods:
We constructed a Markov state transition model to compare the cost-effectiveness of LMWH to VKA therapy for treatment of malignancy-associated thrombosis from a societal perspective. The model had 4 health states: initial anticoagulation, extended anticoagulation, no anticoagulation, and deceased. Cycle-length was 6 months with a lifetime horizon. Potential events in each cycle included recurrent VTE and death from recurrent VTE, major bleeding and death from major bleeding, minor bleeding, and death from other causes. Model inputs for event probabilities, costs, and utility were obtained from previously published literature (e.g., the ONCENOX, Main-LITE, CLOT, CANTHANOX, and CATCH trials); while no specific data exist for the utility of each strategy for treatment of malignancy-associated VTE, we assumed they would be similar to utilities previously published for non-malignant VTE, and performed sensitivity analysis to assess the robustness of our results. Microsimulation of 1000 trials was performed to calculate mean quality-adjusted life-years (QALYs) and costs associated with the two anticoagulation strategies.
Results:
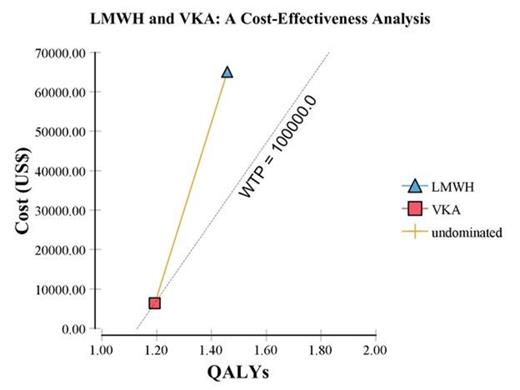
Using a fixed effects model, the meta-analytic estimates of the odds ratio for major bleeding from LMWH as compared to VKA therapy was 0.99 (95% CI 0.65 - 1.50). The odds ratio for recurrent VTE while on LMWH as compared to VKA was 0.55 (95% CI 0.40 - 0.75) in favor of LMWH. The mean cost of the VKA strategy was $6,383.39 (±$5174.56) and for the LMWH strategy it was $64,975.83 (±$3,4743.63). The mean effectiveness of the VKA strategy was 1.19 QALYs (range 0.20 - 7.51); for the LMWH strategy it was 1.46 QALYs (range 0.20 - 9.03), resulting in a mean increase of 0.27 QALYs (Figure). The incremental cost-effectiveness ratio (ICER) was thus $221,281.83 per QALY. One-way sensitivity analysis evaluating the utility of the LMWH strategy from 0 - 1 revealed that VKA was always the preferred strategy at a willingness to pay (WTP) threshold of $100,000 per QALY.
Conclusions:
While LMWH is an effective treatment for malignancy-associated VTE, we found that it offers only a small gain in QALYs compared to VKAs, and that this gain is associated with a significant increase in cost. Our data suggest that LMWH is not a cost-effective strategy when applied to all patients with malignancy-associated VTE and that VKAs may be a reasonable alternative to LMWH.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.