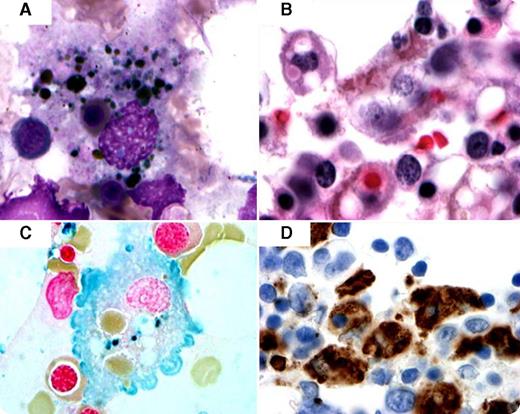
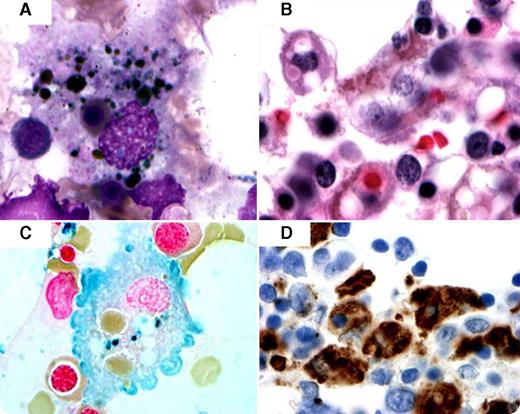
Hemophagocytic lymphohistiocytosis (HLH) is a rare, potentially fatal syndrome despite treatment. It is caused by a dysregulation in natural killer T-cell function, resulting in activation and proliferation of histiocytes with uncontrolled hemophagocytosis and cytokine overproduction. HLH can be either primary, with a genetic etiology, or secondary, associated with malignancies, autoimmune diseases, or infections. There is sparse literature on HLH cases associated with granulomatosis with polyangiitis (GP). Here, we report a 59-year-old woman, with a medical history of GP, chronic anemia, and rapidly progressive glomerulonephritis, who presented with weakness, fatigue, dysuria, cough, and fever with chills for 2 weeks. She developed neutropenia with a white blood cell count of 500/μL and hemoglobin level of 5.1 g/dL, with elevated ferritin levels (>40 000 ng/mL), low haptoglobin level, and increased triglyceride level of 2.66 mmol/L. Bone marrow aspirate and biopsy showed increased histiocytes with intracytoplasmic erythroid precursors, red blood cells, and hemosiderin pigment consistent with hemophagocytic syndrome (panels A-B). Iron stain and CD68 showed histiocytes (panels C-D). The patient was treated with dexamethasone and died within 4 days. Autopsy findings showed arterial thromboemboli with infarcted lungs, liver, and spleen.
The authors report this case to draw attention to this severe syndrome that may often go undiagnosed in patients with rheumatic diseases, especially GP.
Hemophagocytic lymphohistiocytosis (HLH) is a rare, potentially fatal syndrome despite treatment. It is caused by a dysregulation in natural killer T-cell function, resulting in activation and proliferation of histiocytes with uncontrolled hemophagocytosis and cytokine overproduction. HLH can be either primary, with a genetic etiology, or secondary, associated with malignancies, autoimmune diseases, or infections. There is sparse literature on HLH cases associated with granulomatosis with polyangiitis (GP). Here, we report a 59-year-old woman, with a medical history of GP, chronic anemia, and rapidly progressive glomerulonephritis, who presented with weakness, fatigue, dysuria, cough, and fever with chills for 2 weeks. She developed neutropenia with a white blood cell count of 500/μL and hemoglobin level of 5.1 g/dL, with elevated ferritin levels (>40 000 ng/mL), low haptoglobin level, and increased triglyceride level of 2.66 mmol/L. Bone marrow aspirate and biopsy showed increased histiocytes with intracytoplasmic erythroid precursors, red blood cells, and hemosiderin pigment consistent with hemophagocytic syndrome (panels A-B). Iron stain and CD68 showed histiocytes (panels C-D). The patient was treated with dexamethasone and died within 4 days. Autopsy findings showed arterial thromboemboli with infarcted lungs, liver, and spleen.
The authors report this case to draw attention to this severe syndrome that may often go undiagnosed in patients with rheumatic diseases, especially GP.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.