To the editor:
Platelet count has been reportedly associated in a nonlinear way with a number of health outcomes among older subjects1,2 or in high-risk groups.3 One early study has investigated the involvement of platelet count for cardiovascular mortality in a general middle-aged population of healthy men.4
Platelet count decreases during aging, is higher in women than in men,5,6 and varies in populations of different origin.6,7 More recently, it has been reported that platelet count is also influenced by dietary habits.8
A great majority of epidemiologic studies still relies on the use of single reference intervals regardless of age and sex differences in platelet count.9 Similarly, most laboratories in western countries still adopt standard ranges for classification of thrombocytopenia or thrombocytosis (generally 150-400 or 450 × 109 platelets/L for all people).
A recent paper9 provided new data to overcome the use of a single reference interval by identifying age-sex–specific cutoffs derived from a large epidemiologic setting including 3 population-based studies on 40 987 inhabitants of 7 Italian areas.
We aimed to assess the predictive values of these newly defined ranges of platelet count (Table 1) for all-cause mortality.
According to Biino et al,9 low platelet count was defined as platelet number <156 × 109/L or <140 × 109/L for women ≤64 and >64 years of age, respectively; for men, low platelet count was defined as platelet number <141 × 109/L or <122 × 109/L for those ≤64 or >64 years of age, respectively. Cutoffs for high platelet count were set for a platelet count >405 × 109/L or >379 × 109/L for women ≤64 or >64 years of age, respectively; high platelet count was defined as a platelet count >362 × 109/L or >350 × 109/L for men ≤64 or >64 years of age, respectively.
We performed analyses on 24 325 adult individuals ≥35 years of age randomly recruited from the general population of the MOLI-SANI study between March 2005 and April 2010.8,10 Subjects who were not white; had hepatitis, hematologic diseases, missing values for platelet count, and an unreliable medical questionnaire; or were lost to follow-up were not included in the analyses. The final sample consisted of 21 635 subjects.
Blood samples were obtained from participants who had fasted overnight and had refrained from smoking for ≥6 hours. All subjects underwent 1 platelet count measurement. All hemocromocytometric analyses were performed by the same instrument (Coulter HMX; Beckman Coulter, Milan, Italy) within 3 hours of blood collection.
The cohort was followed up until May 2015 with the main outcome of interest being all-cause mortality. The latter was assessed by linkage with Offices of Vital Statistics of the Molise region.
Cox proportional hazard ratios (HRs) with 95% confidence intervals (CIs) were used to assess the association between all-cause mortality and different categories of platelet count with age-sex–specific normal values as the reference category. The multivariable model included age, sex, education, cardiovascular disease, history of cancer, diabetes, hypertension, hypercholesterolemia, leisure-time physical activity, body mass index, smoking, leukocyte count, mean platelet volume, C-reactive protein, hematocrit, use of antiplatelet drugs, and site of recruitment.
During a median follow-up of 7.6 years (interquartile range: 6.7-8.6 years; 163 659 persons/year), 1001 deaths were recorded. The incidence rates and the risk of all-cause mortality among the participants in the different platelet count groups are shown in Table 1.
Compared with the normal range, lower platelet number was significantly related to increased risk of mortality in the multivariable model (HR = 2.17; 95% CI, 1.55-3.05). Conversely, higher platelet count was not associated with higher risk of death (Table 1). A comparison with the usual ranges used for classifying thrombocytopenia and thrombocytosis (platelet count <150 × 109/L or >400 × 109/L, respectively5 ) is also reported in Table 1. According to the standard classification, which does not account for age and sex differences in platelet count, ∼2.9% of the study population would be classified as having thrombocytopenia. At variance, the newly defined ranges in platelet count only identified 1.8% of the population as being at higher risk of death because of low platelet count.
We also found that subjects classified as thrombocytopenic by traditional range intervals (150-400 × 109/L) had a significantly higher risk of all-cause mortality than subjects with normal platelet count or thrombocytosis (HR = 1.62; 95% CI, 1.28-2.05). Compared with subjects included in the normal platelet count category for both criteria, those who shifted from thrombocytopenia, as defined by the usual ranges (<150 × 109/L), to normal platelet count according to the new ranges (n = 278; n of deaths = 50) had a risk of death of 1.37 (95% CI, 1.02-1.85). For comparison, subjects who were considered as having thrombocytopenia according to both classifications (n = 358, n of deaths = 36) had a relative risk of death of 2.22 (95% CI, 1.57-3.13). The number of individuals who shifted from normal values (by traditional ranges) to thrombocytopenia (according to the new ranges) was too small (n = 36, n of deaths = 1; HR = 4.01; 95% CI, 0.56-28.8) to allow any meaningful risk interpretation.
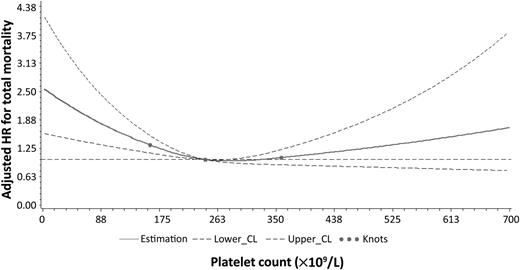
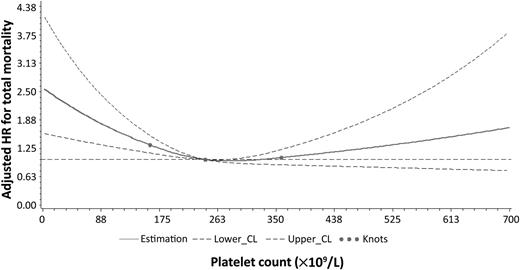
A cubic spline was also generated and showed a U-shaped relationship between platelet number and overall mortality. Findings revealed a nonlinear relationship (P = .0015) with lower platelet count at higher risk for total mortality, in comparison with normal or higher values (Figure 1).
Adjusted HR for all-cause mortality according to platelet count in the MOLI-SANI study population.
Adjusted HR for all-cause mortality according to platelet count in the MOLI-SANI study population.
To the best of our knowledge, this is the first study to test the association of age- and sex-specific ranges of platelet count with risk of all-cause mortality in a large population-based epidemiologic cohort.
Using personalized (sex- and age-specific) rather than traditional reference intervals of platelet count reduces the number/proportion of subjects with thrombocytopenia, as lately observed in a sample of Italian adult patients to whom the newly identified cutoffs were applied.11
The group of possibly true thrombocytopenic subjects (identified by personalized range intervals) had a higher risk of total mortality compared with subjects classified as thrombocytopenic by traditional range intervals.
Strengths of the present study are represented by the large number of subjects and its prospective design. In addition, a large number of possible confounding factors have been considered, including C-reactive protein, mean platelet volume, and use of antiplatelet drugs. A major limitation is the unavailability of cause-specific deaths.
In conclusion, it is suggested that introducing the new platelet count ranges into clinical practice would reduce the number/proportion of normal individuals unduly considered at high risk of all-cause mortality and would be useful to better identify those subjects at higher mortality risk, possibly related to a low platelet count.
The online version of this article contains a data supplement.
Authorship
Acknowledgments: The MOLI-SANI research group thanks the Associazione Cuore Sano Onlus (Campobasso, Italy) for its financial support and the Azienda Sanitaria Regionale del Molise (Campobasso, Italy), the Offices of vital statistics of the Molise region, and the Molise Dati Spa (Campobasso, Italy) for their collaboration and support provided during the follow-up activities.
The enrollment phase of the MOLI-SANI study was conducted at the Research Laboratories of the Catholic University in Campobasso (Italy) and was supported by research grants from Pfizer Foundation (Rome, Italy), the Italian Ministry of University and Research (MIUR, Rome, Italy)–Programma Triennale di Ricerca, Decreto no.1588, and Instrumentation Laboratory (Milan, Italy). The follow-up of the MOLI-SANI cohort is being conducted at the Istituto di Ricovero e Cura a Carattere Scientifico Neuromed (Pozzilli, Italy). M.B. was supported by a Fondazione Umberto Veronesi fellowship. The present analyses were partially supported by the Italian Ministry of Health 2013 (young investigator grant to M.B.; GR-2013-02356060).
Funders had no role in study design, collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the article for publication. All authors were and are independent from funders.
MOLI-SANI study Investigators are listed in supplemental Appendix 1, available on the Blood Web site.
Contribution: L.I., G.d.G., M.B., C.C., M.B.D., and A. Di Catelnuovo contributed to the conception and design of the work and interpretation of data; S.C. and A. De Curtis managed data collection; M.B. and A. Di Castelnuovo analyzed the data; M.B. wrote the paper; and M.B.D., G.d.G., C.C., and L.I. originally inspired the research and critically reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marialaura Bonaccio, Laboratory of Molecular and Nutritional Epidemiology, Department of Epidemiology and Prevention, IRCCS Istituto Neurologico Mediterraneo NEUROMED, Via dell’Elettronica, 86077 Pozzilli (IS), Italy; e-mail: marialaura.bonaccio@neuromed.it.