In this issue of Blood, Spina and coworkers describe the nodal marginal zone lymphoma (NMZL) mutational signature, identifying family links with other marginal zone lymphoma types (NOTCH2, KLF2) and specific mutated genes (PTPRD).1
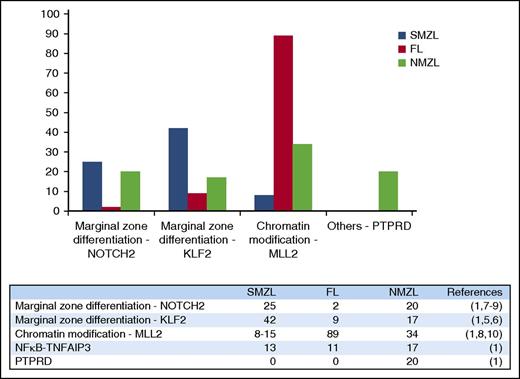
Relative frequency of the most frequently mutated genes in NMZL compared with SMZL and follicular lymphoma (FL).
Relative frequency of the most frequently mutated genes in NMZL compared with SMZL and follicular lymphoma (FL).
NMZL is an infrequent and poorly known B-cell lymphoma type in which the insufficient existing knowledge on its molecular pathogenesis makes identifying specific markers for diagnosis and targeted therapy more difficult.2 NMZL diagnosis relies mainly on the morphological demonstration of marginal zone differentiation, together with the absence of diagnostic markers for other B-cell lymphoma types. Only a pair of molecules (MNDA and IRTA1)3,4 have been proposed as diagnostic markers, whereas B-cell receptor, JAK/STAT, NF-κB, NOTCH, and Toll-like receptor signaling pathways have been proposed to be the main deregulated pathways and potential targets for therapy.2
Now Spina and coworkers have published a next-generation sequencing study with a series of 35 NMZL cases in which nonsilent somatic mutations have been found in MLL2 (34%), PTPRD (20%), NOTCH2 (20%), and KLF2 (17%). NOTCH2 and KLF2 mutations are the hallmark for marginal zone lymphomas and have mainly been found in splenic marginal zone lymphoma (SMZL); both genes have been described as associated with the development of marginal zone B cells in murine models.5-9 Thus, the presence of these mutations in NMZL, a tumor identified by the presence of marginal zone differentiation, makes sense. Less expected is the relatively high incidence of mutations in the MLL2 gene; the lysine methyltransferase MLL2 (also called KMT2D or MLL4) emerges as the most frequently mutated gene in NMZL (34% of cases). When compared with other lymphoma types, MLL2 mutations have so far been mainly found in follicular lymphoma (89%) and diffuse large B-cell lymphoma (32%),10 with a lower frequency in SMZL (8% to 15%)8 (see figure). Differential diagnosis between BCL2-negative follicular lymphoma and NMZL is often a challenging issue; these findings suggest that the borderline between both entities should be reviewed.
Interestingly, Spina and coworkers also identify mutations and deletions of the PTPRD gene, a receptor-type protein tyrosine phosphatase, as enriched in NMZL when compared with SMZL and other B-cell tumors. These PTPRD mutations functionally cause the loss of PTPRD’s phosphatase activity and are associated with deregulation of the cell-cycle transcriptional program and an increased proliferation index.1 This finding, if confirmed by other studies, may facilitate the exploration of the potential heterogeneity of this lymphoma type, reducing the variability in the NMZL diagnosis and eventually making possible a more comprehensive characterization of the molecular alterations driving the growth of this neoplasm.
Conflict-of-interest disclosure: The author declares no competing financial interests.