Abstract
Leukemic relapse after allogeneic hematopoietic cell transplantation (HCT) remains a major cause of treatment failure in patients (pts) who enter HCT with high-risk acute myeloid leukemia (AML). Therapeutic "graft-versus-leukemia" (GVL) effects are often accompanied by substantial morbidity and mortality caused by graft versus host disease (GVHD), as graft T cells have not been selected for specificity for leukemia antigens.
To selectively promote GVL without inducing GVHD, we first developed a therapy employing CD8+ cytotoxic T lymphocyte (CTL) clones targeting Wilms' Tumor Antigen 1 (WT1), a non-polymorphic protein over-expressed 10-1000x by leukemic cells compared to normal CD34+ cells. Although CTL clones derived from HLA matched donors infused in the corresponding pts were safe, the anti-leukemic efficacy was limited in part due to a wide variability of functional avidities obtained for each patient-donor pair and limited persistence of CTL clones (Chapuis A. et al., STM 2013).
We therefore identified and characterized a native, high affinity WT1-specific TCR (TCRC4), isolated from screening the peripheral repertoires of healthy HLA A*0201+ donors. Thus this TCR had been subjected to negative thymic selection, which should minimize the potential risk of off-target toxicity. To enhance persistence, we inserted TCRC4 in EBV- or CMV-specific donor substrate cells, with the former preferred based on the higher frequency of central memory (TCM).
Twenty-two HLA A*0201+ pts received up to 1010 TCRC4 transduced donor-derived virus-specific cytotoxic T cells (CTL)/m2, following recovery of hematopoiesis after a matched HCT transplant for AML (NCT01640301). Adverse events included expected transient (<24 hours) cytokine release syndromes managed on the general ward and transient lymphopenia (<10 days). No evidence of immediate or delayed off-target or on-target/off-tissue toxicity was observed.
Elevenpts with high-risk AML, all of whom had no evidence of disease (NED) at their day 28 post-HCT marrow assessment, received TCRC4-transduced virus-specific CTL (CTLvirus/TCR-C4) on the "Prophylactic Arm" (PA) at a median of 90 days (range 47-190) post-HCT. All 11 pts remain in continued complete remission at a median follow-up of 21.3 months post-HCT. In a matched concurrent cohort of similar high-risk pts who were also NED 28 days post-HCT but did not receive CTLvirus/TCR-C4, 27% had relapsed at 16 months (Figure 1). This suggests the infusion of WT1-specific cells in the post-HCT setting may prevent leukemia recurrence. Although the analysis is still ongoing, preliminary analysis of pts with detectable disease after HCT (11 pts) who received CTLvirus/TCR-C4 on the "Treatment Arm" (TA) revealed evidence of anti-leukemic activity but did not seem to result in a survival advantage compared to matched controls.
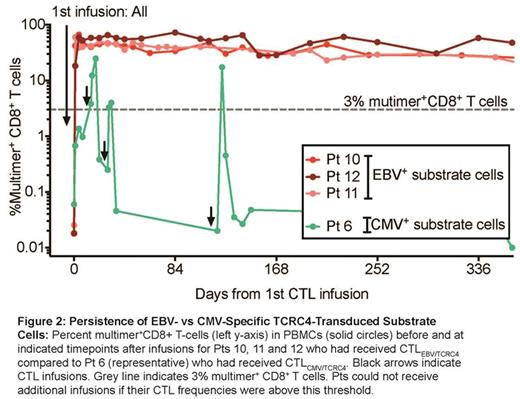
Correlative studies revealed that overall persistence was significantly decreased in the TA, potentially accounting for the lack of survival benefit. Donor-derived CTLEBV/TCR-C4 (11/11 pts on the PA and 7/11 pts on the TA) persisted at higher frequencies (up to 50% of CD8+ T cells for > 1 year) compared to CTLCMV/TCR-C4 (no persistence >3% beyond 7 days)(Figure 2). Analysis of donor virus-specific populations demonstrated that EBV- compared to CMV-specific cells expressed significantly higher long-lived memory and decreased exhaustion/activation markers, supporting results suggesting human cells derived from predominantly TCM populations are imprinted with a program that enhances post-transfer survival.
CTLEBV/TCR-C4 that persisted at high frequencies in the PA not only exhibited an effector phenotype (i.e., did not convert to TCM as had been previously observed) but also expressed Ki67, suggesting continued activation. The transferred CTLEBV/TCR-C4 maintained the ability to secrete IFNg, TNFa and IL-2, preferentially through TCRC4 (Figure 3), and, as no ongoing EBV-reactivation was detected in serum, the results strongly suggest continued WT1-antigen encounter as the driver of proliferation/persistence and a contributing mechanism for AML relapse prevention in the PA. Furthermore, although the infused CTLEBV/TCR-C4 were polyclonal, the dominant clonotypes in the infusion product also composed the majority of persisting cells, suggesting rare "fit" clonotypes expand during cell production and lead to oligoclonal survival in vivo.
Chapuis:Juno Therapeutics Inc: Research Funding. Yeung:Gilead Sciences: Research Funding. Greenberg:Juno Therapeutics Inc: Equity Ownership, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.