Abstract

Background: Limited data exist to describe the clinical features and outcomes for elderly pts with FL. The FLASH group performed a prospectively planned pooled analysis of IPD from first-line RCTs and examined associations between age (<= 70 vs. > 70 years), clinical characteristics and FL outcomes.
Methods: We identified 18 randomized controlled multicenter clinical trials in the FLASH database which enrolled elderly pts (> 70 yrs). From these 18 studies, 5922 previously untreated FL pts were included for this analysis. Complete response (CR) at 24 and 30 months were defined as whether the pt achieved and remains in CR at 24 months and 30 months after initiation of induction treatment. PFS24 is defined as proportion of pts progression-free and alive at 24 months post-randomization. Time to progression (TTP) and overall survival (OS) were defined as time from randomization to the date of progression (censoring for death without progression) and date of death due to any cause, respectively. Progression-free survival (PFS) was defined as time from randomization to the date of progression or death, due to any cause, whichever comes first. Non-lymphoma death was defined as death without prior progression. Early disease outcomes, i.e. CR24, CR30, and PFS24 were primary outcomes; secondary outcomes were TTP, OS, and PFS. For time-to-event outcomes, Kaplan-Meier method and log-rank test were used for univariate estimation and comparison; stratified Cox proportional hazard modeling was used for multivariable analyses. Cumulative incidence methods were used to model PFS while treating disease progression as the primary event of interest and non-lymphoma death as a competing risk. For binary outcomes, multivariable logistic regression was used to estimate the association between age groups and outcomes. Variable adjusted in the regression models are FLIPI score without the age component, ECOG performance status (>= 2 vs < 2), and rituximab use.
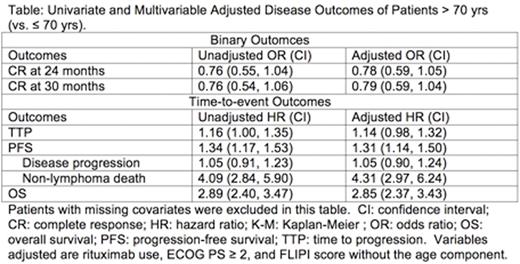
Results: Among 5922 previously untreated FL pts from 18 RCTs, 63% (n = 3728) were <= 60, 28% (n = 1652) 61-70, and 9% (n = 542) > 70 yrs. Pts age > 70 (vs. <= 70) more commonly had elevated LDH (42% vs 36%, p = 0.02), hemoglobin < 12 g/dL (27% vs 19%, p < 0.0001), ECOG PS >= 2 (8.8% vs 5.0%, p = 0.0004), and elevated β2-microglobulin (68% vs 49%, p < 0.001), less often had > 4 lymph nodes involved (54% vs 65%, p < 0.001), and had similar FLIPI scores without age component (p = 0.17). There were no significant differences between groups in: Ann Arbor stage (94% vs 95% stage III/IV) or rituximab use (62% vs 58%). Median survival follow-up was 5.6 yrs. Pts > 70 yrs did not differ from pts <= 70 in rates of CR24 (27% vs 30%, p=0.32), CR30 (29% vs 31%, p=0.55) or PFS24 (63% vs. 67%, p=0.10). Median TTP was 3.8 and 4.0 years for pts > 70 and <= 70, respectively (HR=1.08, 95% CI 0.96-1.23, p=0.20). With a median OS of 14.6 years for all pts, median OS was 7.4 and 15.7 years for pts > 70 and <= 70, respectively (HR=2.35, 95% CI=2.03-2.73, p<0.001). PFS was statistically significantly different but clinically similar at median 3.1 and 3.8 years for pts > 70 and <= 70, respectively (HR=1.26, 95% CI =1.12-1.41, p<0.001). Further investigation showed the difference in PFS was due to higher incidence of non-lymphoma death in pts > 70 with no difference in disease progression (Figure). In regression models, adjusting for rituximab use, ECOG PS >= 2, and FLIPI score without the age component, age > 70 was a significant predictor of OS and PFS (due to higher incidence of non-lymphoma death), but not PFS24, CR24 or CR30 (Table).
Conclusions: FL pts > 70 yrs treated on trials have similar early disease outcomes to younger patients. There is no disease-specific outcome difference between age groups. Age alone should not disqualify patients from standard treatments or RCTs.
Flowers:Genentech: Consultancy, Research Funding; NIH: Research Funding; Mayo Clinic: Research Funding; TG Therapeutics: Research Funding; Millenium/Takeda: Research Funding; ECOG: Research Funding; Acerta: Research Funding; Pharmacyclics, LLC, an AbbVie Company: Research Funding; Roche: Consultancy, Research Funding; AbbVie: Research Funding; Infinity: Research Funding; Gilead: Consultancy, Research Funding. Ou:Mayo Clinic: Employment. Shi:Mayo Clinic: Employment. Hochster:Genentech: Consultancy, Other: Consultancy fees for advisory boards for GI cancer and bevacizumab with amounts within Yale University de minims guidelines. Brice:Roche: Honoraria; Takeda Pharmaceuticals International Co.: Honoraria, Research Funding; Bristol Myers-Squibb: Honoraria; Gilead: Honoraria; Seattle Genetics: Research Funding. Hiddemann:Roche: Other: Grants; Roche: Membership on an entity's Board of Directors or advisory committees; Genentech: Other: Grants. Marcus:Takeda: Consultancy, Speakers Bureau; Roche: Consultancy, Speakers Bureau. Kimby:Abbvie: Consultancy, Honoraria; Jansen: Consultancy, Honoraria; Celgene: Honoraria; Baxalta: Consultancy; Gilead: Honoraria. Herold:Gilead: Other: Personal fees from member advisory board; Celgene: Honoraria; Genentech: Other: Grants; Roche: Honoraria, Other: Grants. De Bedout:Celgene: Employment. Nielsen:Hoffmann-La Roche: Employment. Morschhauser:Roche: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Servier: Consultancy, Honoraria; Gilead Sciences: Consultancy, Honoraria; Janssen: Honoraria. Rummel:Mundipharma GmbH: Other: Personal fees, Research Funding; Roche Pharma AG: Other: Personal fees, Research Funding. Vitolo:Gilead: Other: Honoraria for lectures; Takeda: Other: Honoraria for lectures; Roche: Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures; Janssen: Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures. Salles:Celgene: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Gilead: Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Roche/Genentech: Consultancy, Honoraria, Research Funding; Mundipharma: Honoraria. Sargent:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract