Abstract
Background: Vitamin D insufficiency (VDI) has been associated with inferior outcomes in patients with follicular lymphoma (FL) treated with chemotherapy and an anti-CD20 monoclonal antibody (immunochemotherapy; IC), but whether this association holds for other FL treatment strategies is not known. Furthermore, the subset of FL patients who experience clinical failure (progression, treatment failure) within 12 months of diagnosis have an inferior outcome compared to those achieving event-free status at 12 months (EFS12). We tested the hypothesis that VDI is predictive of early clinical failure (failure to achieve EFS12), overall survival (OS), and lymphoma-specific survival (LSS) among FL patients overall and in subgroups who were initially observed, treated with IC, rituximab monotherapy, or other therapies.
Methods: We evaluated this hypothesis in a prospective cohort study of 642 newly diagnosed patients with grade 1-3a FL enrolled from 2002-2012 in the Molecular Epidemiology Resource of the Iowa/Mayo Lymphoma SPORE. Serum 25-hydroxyvitamin D [25(OH)D] was measured by liquid chromatography-tandem mass spectroscopy, and VDI was defined as serum total 25(OH)D <20 ng/mL (per Institute of Medicine criteria) determined within 120 days of diagnosis. We used logistic regression to estimate Odds Ratios (ORs) and 95% confidence intervals (CIs) and Cox regression to estimate hazard ratios (HRs) and 95% CIs. We adjusted for FLIPI, body mass index, and month of blood draw; for the full cohort, we additionally adjusted for treatment.
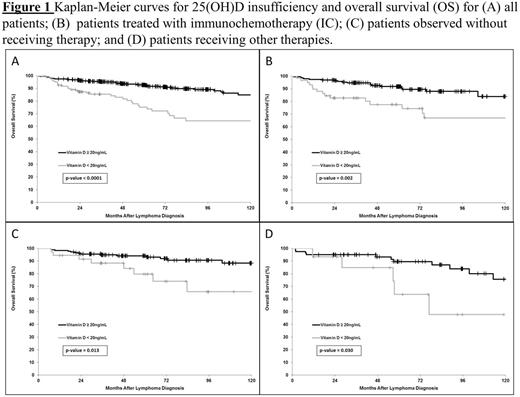
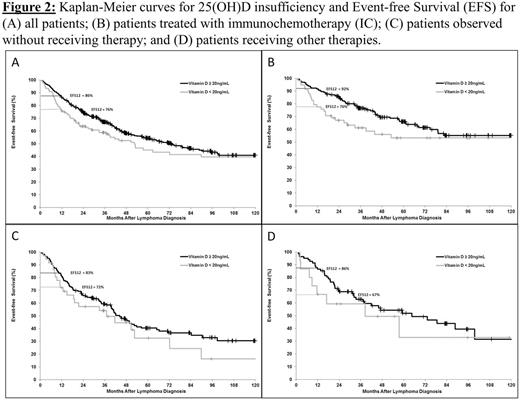
Results: The mean age at diagnosis was 60 years (range 23-93); 19% of patients had VDI. The median follow-up period was 59 months (range 1-144), with 297 events and 78 deaths (42 due to lymphoma). Treatment included IC (N=252), observation (N=218), rituximab monotherapy (N=76), or other (N=96). OS and EFS curves are shown in figures 1 and 2. In the full cohort, VDI was associated with inferior EFS12 (OR=2.05; 95% CI 1.18-3.54), OS (HR=2.35; 95% CI 1.37-4.02), and LSS (HR=2.97; 95% CI 1.52-5.80). In the IC subset, VDI was associated with inferior EFS12 (OR=3.00; 95% CI 1.26-7.13), OS (HR=2.86; 95% CI 1.39-5.85), and LSS (HR=2.96; 95% CI 1.29-6.79). VDI was associated with inferior OS in patients who were observed (HR=2.25; 95% CI 1.20-6.76) or received other therapies (HR=3.06; 95% CI 1.01-9.24). VDI was positively but not statistically significantly associated with inferior EFS12 in the patients who were observed (OR=1.71; 95% CI 0.70-4.17) or received other therapies (OR=2.31; 95% CI 0.41-13.07), with low power for these associations; LSS could not be estimated due to lack of deaths. There were too few events (N=10) and deaths (N=5) in the R-monotherapy group for analysis.
Conclusions: We confirm previous findings that vitamin D insufficiency is associated with adverse long-term prognosis among patients with FL treated with IC, and extend these findings to patients who are initially observed or treated with other therapies. For the first time, we observed an association of vitamin D insufficiency with early clinical failure, suggesting a potentially modifiable factor to address in this subset of patients with poor outcomes. Whether treating VDI improves outcomes in FL warrants assessment.
Ansell:BMS, Seattle Genetics, Merck, Celldex and Affimed: Research Funding. Nowakowski:Celgene: Research Funding; Morphosys: Research Funding; Bayer: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.