Abstract
Background
Current guidelines recommend all cancer inpatients receive pharmacologic VTE prophylaxis in the absence of contraindications. This is extrapolated from trials showing the benefit of VTE prophylaxis in general medical inpatients and the known increased risk of VTE in cancer patients. However, given the increased risk of bleeding in cancer patients on anticoagulation (AC), it is vital to better define a subpopulation of cancer inpatients who most benefit from VTE prophylaxis. Current inpatient VTE risk models, including Padua, Caprini and IMPROVE, contain cancer as a variable and thus are not discriminative among cancer patients. Although the Khorana score (KS) stratifies VTE risk by cancer type, it was originally derived for cancer outpatients, and has yet to be validated for inpatients. Using a large multi-center cohort, we developed a novel VTE risk assessment model (RAM) specific to cancer inpatients, the CANclot score.
Methods
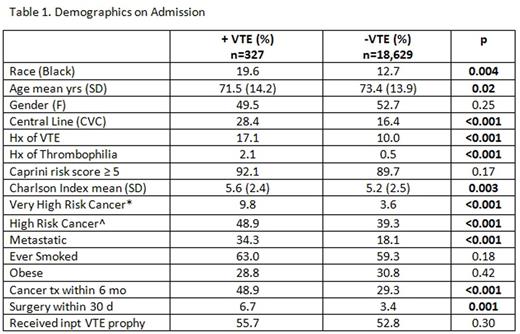
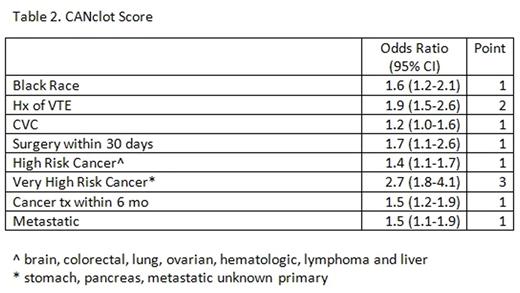
The Michigan Hospital Medicine Safety Consortium, a 49 hospital collaborative, established a multicenter retrospective cohort of medical inpatients > 18 years of age. Exclusion criteria include surgical patients, pregnancy, admission to the ICU or for palliative care, therapeutic AC, diagnosis of acute VTE, history of VTE within 6 months, and length of stay < 2 days. Patient demographics, clinical characteristics, and VTE events (both hospital associated and 90 day post discharge) were recorded. The CANclot risk assessment model was derived from logistic regression analyses of an apriori list of risk factors. Significant risk factors included in the CANclot scale were weighted based on the respective odds ratio estimates and an optimal cut-off was chosen. Model discrimination of the CANclot score was compared with other published risk models.
Results
Between 7/2012-7/2015, 18,956 cancer admissions were included. 2,464 (13%) had a pre-defined contraindication to prophylaxis (active bleed within 3 months, coagulopathy, or high risk brain metastasis). Of all admissions, 52.8% received VTE prophylaxis. A total of 327 (1.7%) VTE events were observed; 51/327 (15.6%) VTE events occurred during admission and 276/327 (84.4%) within 90 day f/u.
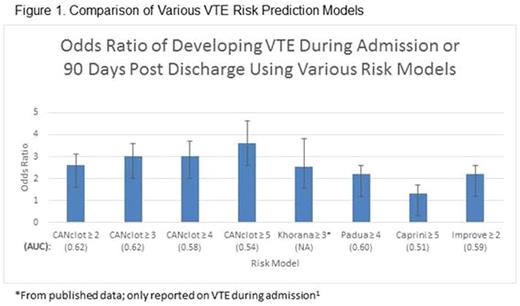
When comparing AUC's of different risk models, CANclot ≥ 3 was superior to Padua ≥ 4 (p=0.01), Caprini ≥ 5 (p=0.01) and IMPROVE ≥ 2 (p=0.02). In our dataset 4,695 (25%) of patients had a CANclot score ≥ 3.
Conclusion:
The CANclot score is a novel VTE risk assessment tool derived specifically for cancer inpatients. Compared to other published risk prediction tools used in the general population, CANclot ≥ 3 shows an improved predictive ability for VTE and good yield, applying to 25% of the population.
Improving VTE prediction in hospitalized cancer patients is crucial because targeting only those at highest risk may spare low risk patients from untoward bleeding complications from AC. Additionally, we found the majority of VTE events occurred during the 90 day followup period which calls for further attention to the possible need for extended prophylaxis in this population. Limitations to our study include a low overall rate of VTE, lack of some cancer specific variables, and that risk score values have not yet been corrected for optimism. The CANclot VTE risk score is a promising new tool for cancer inpatients that warrants further validation.
1 Patell R et al. JCO 34, 2016 (suppl; abstr 6598)
Flanders:Blue Cross Blue Shield: Research Funding; Wiley Publishing: Patents & Royalties. Sood:Bayer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.