Abstract

INTRODUCTION:
Thromboprophylaxisduring hospitalization is an accepted intervention to prevent hospital related venous thromboembolism (VTE), however VTE still occurs post discharge. Recently, several randomized trials have compared extended prophylaxis with a direct oral anticoagulant (DOAC) for a prolonged period after hospital discharge to standard short-course prophylaxis with low molecular weight heparin (LMWH) in acutely-ill medical patients. While DOACs offer a convenient means to prevent post-hospitalization VTE, it remains unclear if this intervention has a positive risk-benefit ratio in the overall population of acutely hospitalized medical patients. To better answer this, we performed the following systematic review and meta-analysis.
METHODS:
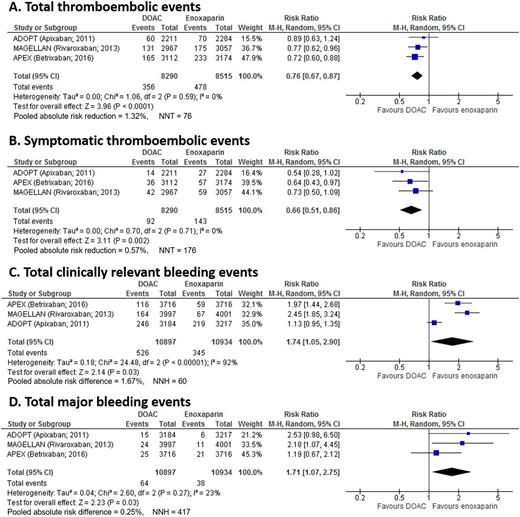
We performed a systematic literature search in Medline using PUBMED in an attempt to identify all relevant randomized clinical trials comparing extended prophylaxis with any DOAC to standard course prophylaxis in hospitalized medical (non-surgical) patients. We extracted data on study design and characteristics, total VTE, symptomatic VTE, total bleeding, and major bleeding. Pooled relative risk (RR) was calculated with a corresponding 95% confidence interval (CI) using a Mantel-Haneszelrandom-effects model. Absolute risk differences and the number needed to treat (NNT) or number needed to harm (NNH) were generated along with Forest plots.
RESULTS:
Our search identified 338 individual publications, of which 313 were excluded on initial screening by title and abstract. Full text were obtained of the remaining 25 studies and independently reviewed by two physicians, of which 22 were excluded for the following reasons: Comments on other articles (12), Study Protocol (1), Review article (8), Data unavailable (1).
A total of three trials, enrolling 22,142 patients, were included. Apixaban, rivaroxaban, andbetrixabanwere each evaluated by one study. Among the studies, 11,064 patients were randomized to extended DOAC prophylaxis, while 11,078 were randomized to standard course LMWH prophylaxis.
In pooled analysis, VTE (including screened asymptomatic VTE) occurred in 4.30% of the patients receiving extended DOAC prophylaxis and 5.61% of patients treated with standard course LMWH (RR 0.76 [95% CI, 0.67-0.87], P = <0.0001, I2 = 0%). The NNT was 76. Symptomatic VTE occurred in 1.11% of patients treated with extended course DOACs and 1.68% patients treated with standard course LMWH. DOAC extended prophylaxis was associated with a significant reduction in symptomatic VTE (RR 0.66 [95% CI, 0.51-0.86], P = 0.002, I2 = 0%). The pooled absolute risk reduction was 0.57%, with a NNT of 176.
A bleeding event occurred in 4.82% of patients receiving extended course DOACs compared to 3.16% of patients receiving standard course LMWH. The pooled analysis demonstrates a statistically relevant increase in bleeding (RR 1.74 [95% CI, 1.05-2.90], P < 0.001, I2 = 92%), with an absolute risk difference of 1.67% and a NNH of 60. A major bleeding event occurred in 0.59% of patients treated with extended course DOACs and 0.35% of patients treated with standard course LMWH. DOAC extended prophylaxis was associated with a significantly increased rate of major bleeding (RR 1.71 [95% CI, 1.07-2.75], P = 0.03, I2 = 23%). The pooled absolute risk difference is 0.24% with a NNH of 417.
CONCLUSIONS:
In this pooled analysis, extendedthromboprophylaxiswith DOACs was associated with a significant decrease in total and symptomatic VTEin medical patientsas compared to standard course LMWH. However, the low rate of symptomatic VTE, low absolute risk reduction, and significantly increased rate of bleeding with extended prophylaxis calls into questions if this intervention should be used.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract