Abstract
Introduction: In the Nordic Lymphoma Group trial NLG T-01, patients with newly diagnosed peripheral T-cell Lymphoma (PTCL) were treated with six courses of CHOEP (up to 60 yrs) or CHOP (61-67 yrs) followed by high-dose chemotherapy (BEAM) and autologous stem cell transplantation (ASCT). At 5 years median follow-up, the progression-free survival of the trial cohort was 44%. On this background, the NLG-T01 treatment strategy has become the recommended first-line treatment for younger fit patients in the Nordic countries and in the latest ESMO guidelines for PTCL. Despite this intensive approach with up-front ASCT a fraction of patients still relapses. In an attempt to find factors predictive for survival after up-front ASCT we aimed to analyze the impact of radiologic response at the first interim evaluation on long-term survival.
Methods: All NLG T-01 patients (TrialP) with "nodal" PTCL, i.e. anaplastic large cell lymphoma, ALK-negative (ALCL), angioimmunoblastic T-cell lymphoma (AITL) and peripheral T-cell lymphoma not otherwise specified (PTCL NOS), that actually received the planned ASCT were included. Using national (Sweden and Denmark) or site-specific (Finland and Norway) registries, additional patients (RegP) who received the same treatment schedule, but off-protocol, were identified, and data for these patients was collected retrospectively. Overall survival (OS) was calculated from date of stem cell reinfusion until death from any cause. The first interim computed tomography (iCT) scan was performed after 3 cycles of chemotherapy. Response assessment in the NLG-T-01 trial was based on the 1999 International Working Group criteria for response, which allowed for complete remission unconfirmed and these patients have been grouped with CR in the present analysis. Progressive Disease (PD) was defined as increase of ≥25% of any lesion.
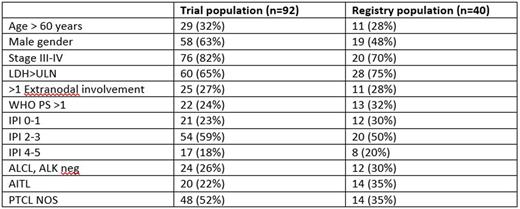
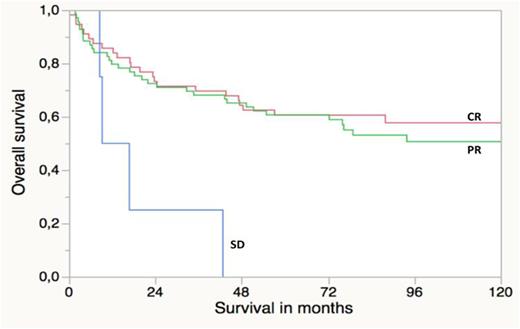
Results: Altogether, 132 patients were included in the present study (TrialP n= 92; RegP n=40). The clinical characteristics are presented in the Table. The 5-year OS among all the patients was 58%. Response at iCT was CR, partial remission (PR) and SD in 44%, 53% and 3% respectively. Of the four patients with SD at iCT, all four patients attained PR after completing six cycles of chemotherapy prior to ASCT. Kaplan-Meier estimates for OS are illustrated in the Figure and the 5-year OS was identical, 61%, for patients in CR and PR but 0%for patients with SD. Using log-rank comparisons patients achieving SD at iCT had a significantly worse survival compared to patients with CR or PR (p=.01).
Discussion: This study is to our knowledge the first to analyze whether interim treatment response can predict long-term OS in "nodal" PTCL patients treated with CHOEP or CHOP consolidated by up-front ASCT. Patients with SD after three cycles of chemotherapy had a very poor survival compared to patients with PR or CR. This was an expected finding, and it confirms the importance of chemo-sensitive disease as a necessary pre-requisite in order to benefit from up-front high-dose consolidation. Using CT, there was no survival difference between patients with CR or PR at the first interim evaluation. A larger cohort might reveal further differences in subgroups, particularly if PET/CT based remission evaluation should confirm itself as a useful tool also in nodal PTCL. At present our study indicates that failure to achieve PR after three cycles of CHOEP/CHOP identifies patients at high risk of relapse/progression that are in need of a different therapeutic strategy than continuing with CHOEP/CHOP towards an ASCT.
Mannisto:Gilead: Other: Travel expenses; Celgene: Other: Travel expenses; Novartis: Other: Travel expenses; Amgen: Other: Travel expenses; Takeda: Honoraria, Other: Travel expenses; Roche: Honoraria, Other: Travel expenses; Pfizer: Honoraria; SOBI: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.