Abstract
Background: International Prognostic Index (IPI) has been used as the primary prognostic tool in diffuse large B cell lymphoma (DLBCL) for more than 20 years. Even though the disease is more common in older population, the impact of comorbidities, dose reductions, and treatment-related adverse events (AEs) on the outcome in elderly DLBCL patients has not been well established. In this study, we aimed to investigate the effect of IPI, clinicopathological features, Charlson Comorbidity Index (CCI), AEs and dose reductions on survival of DLBCL patients aged 60 years or above.
Methods: We identified 910 DLBCL patients (pts) treated at Cleveland Clinic between 2004-2014 and this analysis includes 413 pts aged ≥60 years. Patient and disease characteristics and treatment data of pts who received at least one cycle of treatment were analyzed for prognostic significance. CCI was calculated, excluding lymphoma, and patients were divided into low CCI (CCI score of 0-2) or high CCI (≥3). For regression analysis, patients were grouped into good or poor risk based on IPI ≤ 2 vs 3-5.
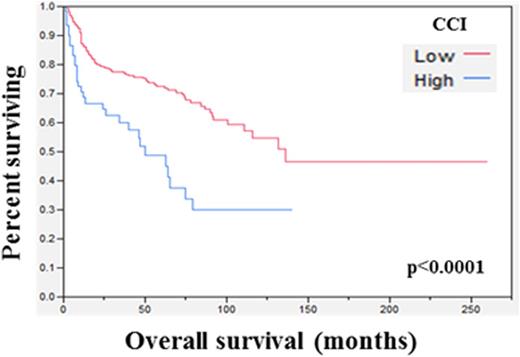
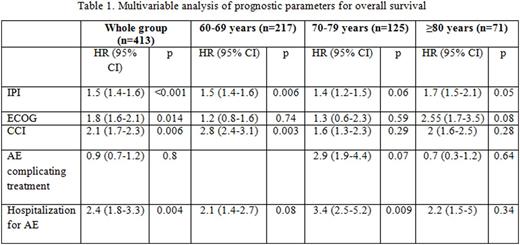
Results: Median age of our cohort was 69 years (range, 60-100), 55% were male, and 91% Caucasian. Pts were divided into 3 age groups; 60-69 yrs (N=217), 70-79 yrs (N=124) and >80 yrs (N=72). Most pts had advanced stage disease (59%), high IPI ≥3 (58%) good performance status (PS) ≤1 (74%), and no B symptoms (31%). 15% had high CCI (≥3) with a trend towards higher incidence in >80 yrs (p=0.05). Our cohort had predominantly germinal center (GC) DLBCL (60%) with low incidence of MYC translocation (28%) among the 89 pts tested. Only median BMI (28%, p=0.007) and performance status (≥2: 27%, p=<0.001) was statistically significant among the age grps. 85% were treated with R-CHOP, 2% received CHOP, and 3% received R-EPOCH. 70% experienced at least one clinically significant AE with infection (34%) and febrile neutropenia (31%) being common. 78% had dose reduced chemo with higher frequency seen in older pts (59% in >80 yrs) (p=<0.001). Overall response rate was 92% with 78% achieving CR and no difference among the groups. Median OS and PFS were 9.6 and 3.8 years respectively with an estimated 10 year OS and PFS of 50% and 30%. In the univariable analysis, IPI (OS: HR 1.7, p=<0.001; PFS: HR 1.39, p=<0.001), ECOG PS (OS: HR 2.94 p=<0.001; PFS: 2.29, p=<0.001), CCI (OS: HR 2.1, p=<0.001; PFS: HR 1.59, p=0.015), LDH ratio (OS:HR 1.53, p=0.008; PFS: HR 1.58, p=<0.001), chemotherapy dose reduction (OS: HR 1.64, p=0.016; PFS: HR 1.45, p=0.029), AE (OS: HR 1.78, p=0.17; PFS: 1.56 p=0.017), and hospitalization (OS: HR 4.01, p-=<0.001; PFS: HR 1.56, p=0.017) predicted inferior OS and PFS. On multivariable analysis, only IPI (HR 1.5, p<0.001), CCI (HR 2.1, p=<0.006) and hospitalization (HR 2.4, p=<0.004) were significant predictors of OS. In addition to CCI (HR 2.0 p=0.013) and hospitalization (HR 2.45 p=<0.001), B symptoms (HR 0.62, p=0.038) was also prognostic for PFS. Among the age groups, adverse risk factors for OS were IPI (HR 1.47, p=0.006) and CCI (HR 1.47, p=0.006) in 60-69 yrs, and hospitalization in 70-79 years (HR 3.42, p=0.009). None of these factors predicted survival in >80 yrs, although there was trend observed with IPI (p=0.058) and PS (0.052).
Conclusion: In this single center large cohort of DLBCL pts, higher CCI and hospitalization for AE were significant predictors of decreased OS and PFS, especially in pts aged 60-69 years. Although IPI is predictive, a better prognostic model incorporating comorbidities and treatment toxicities may help to better risk stratify older DLBCL patients.
Smith:Spectrum: Honoraria; Abbvie: Research Funding; Genentech: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.