Abstract
Introduction: The prognostic relevance of age at diagnosis has long been recognized in DLBCL. Its role in the biology of disease has not been clarified, and it has been postulated that the worse prognosis of older DLBCL patients is a result of more aggressive disease combined with poor tolerance to aggressive therapy. The introduction of rituximab has improved the outcomes of DLBCL in all ages, whereas reduced dose and anthracycline-free regimens have improved access of elderly patients to more effective DLBCL therapy.
Methods: We accessed the Hematologic Malignancies database of University Hospitals Seidman Cancer Center for DLBCL patients diagnosed between 2002 and 2014. Information collected included demographic as well as baseline laboratory and disease characteristics. Relapse and overall survival times were calculated from end of therapy and time of diagnosis, respectively, using the Kaplan Meier method, comparisons were done using the log-rank test. Cumulative incidence of major cardiovascular events (including myocardial infarction, coronary artery disease without infarction, congestive heart failure and arrhythmias) were calculated using death as competing risk; comparisons between groups were done using the Gray test.
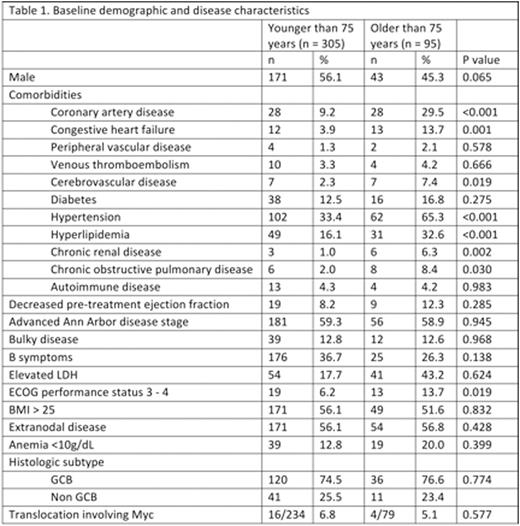
Results: A total of 400 DLBCL patients were identified, 95 were older than 75 years. Table 1 shows the baseline demographic and disease characteristics. Older patients had a higher incidence of comorbidities and higher rates of decreased performance status. There were no other differences in baseline disease characteristics. A smaller proportion of older patients proceeded to receive antineoplastic therapy (81% vs. 91%, p = 0.002). Therapy for older subjects was less intense (full dose R-CHOP 54.5% vs. 81.1%, p<0.001) with more planned and unplanned dose reductions (48% vs. 11%, p<0.001). Despite less intense therapy, response rates were not statistically different between the two age groups (84% vs. 87%, p = 0.687).
After a median of 28 months follow up, estimated 3-year overall survival was 51% (95% CI 40-61.8%) for patients >75 years vs. 76% for younger patients (95% CI 70.6-80.9%)(p<0.001). In patients who received therapy (n=77 older than 75 years; n=281 for < 75 years), there was no difference in relapse-free survival from the start of treatment (3-year RFS: 77% (95% CI 66.5-88.5%) for patients > 75 years and 65% (95% CI 59.1-71.6%) for younger patients, p=0.155). The cumulative incidence (CI) of cardiovascular events, with death due to any other cause as a competing risk, was higher in subjects >75 years: 1-year CI was 15.3% vs. 7.6% in younger patients (p = 0.04).
Conclusions: DLBCL patients older than 75 years have a higher mortality risk following DLBCL diagnosis than younger patients, despite having similar response rates and relapse free survival. While chemotherapy dose reduction does not appear to affect disease control, high rates of cardiovascular events suggest future studies should focus on the minimization of short and long term toxicities of therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.