Abstract

Background: The 2016 revision to the World Health Organization (WHO) classification of myeloid neoplasms has recommended distinction between "proliferative" (WBC ≥ 13 x 10(9)/L) and "dysplastic" (WBC < 13 X 10(9)/L) subtypes of chronic myelomonocytic leukemia (CMML). In the current study of 261 molecularly-annotated cases, we sought to clarify the prognostic relevance of distinguishing proliferative from dysplastic CMML and also describe differences in the distribution of disease-associated mutations.
Methods: 261 patients with WHO-defined CMML were included in the study. All patients had bone marrow (BM) biopsies and cytogenetics performed at diagnosis. Targeted capture assays were carried out on BM DNA specimens obtained at diagnosis for the following genes; TET2, DNMT3A, IDH1, IDH2, ASXL1, EZH2, SUZ12, SRSF2, SF3B1, ZRSR2, U2AF1, PTPN11, Tp53, SH2B3, RUNX1, CBL, NRAS, KRAS, JAK2, CSF3R, FLT3, KIT, CALR, MPL, NPM1, CEBPA, IKZF, and SETBP. The 2016 WHO criteria were used to sub-classify CMML into proliferative and dysplastic subtypes.
Results:Among the 261 study patients, 65% were males and median age was 70 years. 154 (59%), 64 (25%) and 43 (16%) patients were classified as CMML-0, 1 and 2, respectively. At a median follow-up of 23 months, 174 (67%) deaths and 37 (14%) leukemic transformations were documented. Mutational frequencies were; TET2 45%, ASXL1 45%, SRSF2 40%, NRAS 14%, SETBP1 13%, CBL 10%, JAK2 7%, RUNX1 6%, U2AF1 6%, DNMT3A 6%, SF3B1 5%, ZRSR2 4%, Tp53 4%, IDH2 4%, KRAS 3%, PTPN11 2%, SH2B3 1%, CSF3R 1%, IDH1 1%, EZH2 1%, SUZ12 1%, KIT 1%, FLT3 1%, and CALR 1%. Risk stratification was based on the Mayo Molecular Model: 31% high, 30% intermediate-1, 28% intermediate-2 and 11 % low risk.
i) Dysplastic versus proliferative CMML: phenotypic and molecular differences
139 (53%) patients had proliferative and 122 (47%) dysplastic subtypes. There was no difference between the CMML subtypes in terms of age and gender distribution, hemoglobin level, platelet count or BM blast content. Patients with proliferative CMML had higher absolute monocyte counts (AMC) (p<0.0001), circulating immature myeloid cells (IMC, p<0.001), circulating blasts (p<0.001) and serum LDH levels (p=0.01). The following gene mutations were more common in proliferative vs dysplastic CMML: ASXL1 (54% vs 37%, p=0.009), JAK2 (11% vs 3%, p=0.01) and CBL (11% vs 8%, p=0.047); SF3B1 mutations were more common in dysplastic CMML (8% vs 1%, p=0.02). There was no difference in the incidence of TET2, DNMT3A and SRSF2 mutations whereas there was a trend towards a higher prevalence of NRAS (p=0.06) and CSF3R (p=0.06) mutations in proliferative CMML. Cytogenetic abnormalities (p=0.03), including higher risk categories by the Spanish (p=0.03) and the Mayo-French (p=0.01) systems were more common in proliferative CMML.
ii) Impact on overall and leukemia-free survival:
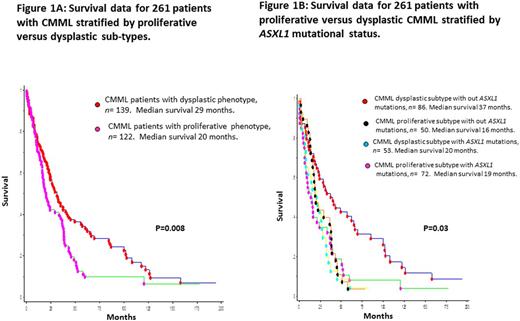
Median survival for the entire cohort (n=261) was 24 months. In univariate analysis, survival was shorter in patients with proliferative (median 20 months) versus dysplastic (median 29 months) CMML (p=0.008; HR1.5, 95% CI 1.1-2.1; Figure 1A). Other variables of significance, in univariate analysis, included hemoglobin (p=0.001), leukocyte count (p=0.001), AMC (p=0.003), PB blast % (p=0.003), IMC (p=0.01), BM blast % (p=0.045), abnormal karyotype (p=0.02), ASXL1 (p=0.01) and DNMT3A (p=0.0003) mutations. In multivariable analysis, the difference in survival between proliferative and dysplastic subtypes remained significant with the addition of hemoglobin level (p=0.01), PB blast % (p=0.02), IMC (p=0.04), BM blast % (p=0.01) or DNMT3A mutations (p=0.01). This was, however, not the case with addition of leukocyte count (p=0.32), AMC (p=0.18) or ASXL1 mutational status (p=0.14); whereas the adverse impact on survival from the latter three parameters remained significant. The prognostic impact of ASXL1 mutations was most apparent in dysplastic CMML (Figure 1B). There was no difference in leukemic transformation rates (p=0.4).
Conclusions: In the context of current prognostic models, sub-classification of CMML into proliferative and dysplastic subtypes might not provide additional prognostic value. The apparent difference in survival between the two subtypes of CMML is probably accounted for by the higher prevalence of leukocytosis/monocytosis and of ASXL1 mutations in proliferative CMML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract