Abstract
Regulatory T cells (Tregs) possess the ability to suppress chronic graft-versus-host disease (cGVHD). Hence, the in vivo expansion of Tregs can be used as therapy against cGvHD. In addition to IL-2, Tregs require TCR and costimulatory signals from antigen presenting cells such as dendritic cells (DCs) for their optimal proliferation. Both fms-like tyrosine kinase 3 ligand (FLT3L) and granulocyte-macrophage colony stimulation factor (GM-CSF) induce the development of DCs and promote the proliferation of Tregs in a DC-dependent manner. GM-CSF preferentially increases CD11c+CD8a- DCs, whereas FLT3L more equally supports the development of many DC subsets. However, it is unknown whether GM-CSF-mediated CD11c+CD8a- DC expansion leads to the proliferation of Tregs and contributes to the inhibition of alloimmune responses against host antigens.
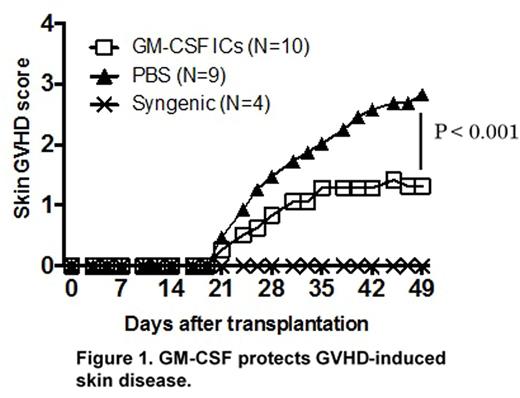
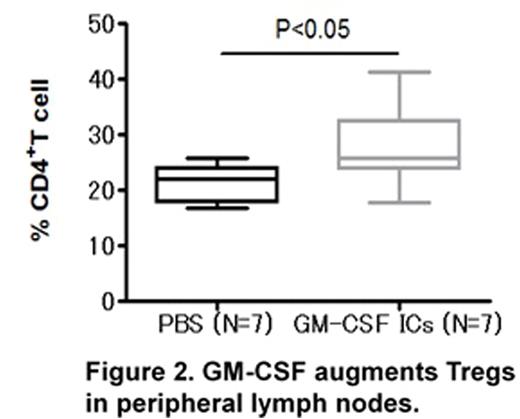
To test whether the injection of GM-CSF augments Tregs and ameliorates cGVHD, we used a MHC-matched mouse cGVHD model (B10.D2 → Balb/c). Balb/c mice were lethally irradiated (850 cGy) and transplanted with 8 × 106 T cell-depleted bone marrow cells and 3.5 × 106 CD4+ T cells from either syngeneic or B10.D2 mice. Host mice were treated with vehicle or GM-CSF (in the form of immune complexes; GM-CSF ICs) for 3 days (days 17-19) and monitored for skin GVHD score and mortality. We used GM-CSF ICs because the injection of GM-CSF ICs but not GM-CSF itself increased splenic CD11c+CD8a- DCs and Tregs. The administration of GM-CSF to allogeneic host mice significantly protected against GVHD-induced skin diseases (p<0.001) (Fig 1). Similar results were obtained when GM-CSF ICs were administrated at a later stage (days 27-29). Although CD11c+CD8- DCs were decreased in mice transplanted from the allogeneic donor compared with mice transplanted from the syngeneic donor, the administration of GM-CSF increased the CD11c+CD8a-/CD11c+CD8a+ DC ratio. However, the expansion of macrophages was not observed in mice administered GM-CSF. Expectedly, the administration of GM-CSF increased Tregs in the peripheral blood and the peripheral lymph nodes (PLNs) (P<0.05) (Fig 2). We investigated the production of proinflammatory cytokines (IFN-g, IL-17) of CD4+ T cells in the spleen, PLNs, and the skin by intracellular cytokine staining, as these cytokines are important for cGVHD pathogenesis in this model. The proportion of IFN-g+CD4+ T cells in the spleen and PLNs was slightly but not significantly decreased in GM-CSF-administered mice. The proportion of IL-17+CD4+ T cells in the skin was decreased in GM-CSF-administered mice compared to vehicle-administered mice. We next investigated the production of IL-2 and IL-10, as these cytokines are associated with survival and function of Tregs. Skin infiltrating Tregs were not increased in GM-CSF-administered mice compared to vehicle-administered mice; however, the proportion of IL-10+ Tregs was increased in GM-CSF-administered mice. The proportion of IL-2+CD4+ T cells was comparable in the allogeneic host with or without GM-CSF, indicating that GM-CSF-induced Treg expansion did not result from an increase in IL-2 production by CD4+ T cells. Together, these data suggest that GM-CSF induces the proliferation of Tregs by expanding CD11c+CD8a- DCs, and can regulate alloimmune responses in a cGVHD mouse model. Our findings indicate the potential of GM-CSF as a therapeutic strategy to ameliorate cGVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.