Background
Infections are potential life-threatening complications during profound neutropenia in patients undergoing high dose chemotherapy with autologous stem cell transplant (HDC-ASCT). The current standard of practice is to start empiric broad spectrum antibiotics as soon as the patient becomes febrile.
However, patients undergoing transplant also develop fever due to engraftment. Fever in this case is non-infectious and rather related to cytokine release from newly engrafted cells. Indeed, patients with engraftment syndrome experience signs of capillary leakage such as lung infiltrates, swelling, edema and generalized papule-macular erythema. Within this setting fever is always present.
In our institution we made the observation that a significant number of patients develop acute kidney injury (AKI) when treated with vancomycin during the engraftment period. Perhaps renal hypo-perfusion due to fluid shifting during engraftment makes these patients more susceptible to drugs with a nephrotoxic profile, such as vancomycin.
The objective of the current study was to identify the incidence, predictors and outcome for AKI in patients who received HDC-ASCT and were treated with Vancomycin during the engraftment period. Close monitoring of fluid status to maintain an adequate renal perfusion may prevent kidney injury during this time.
Methods
The study population consisted of patients who underwent HDC-ASCT from January 2011 to December 2013 at the Audie L. Murphy Memorial Veterans Hospital. Only patients who developed fever during the time of engraftment where included. Rising of baseline creatinine from the time of fever was compared between those who receive vancomycin and the group who did not. Both groups were comparable and matched for age, race and diagnosis. The development of acute kidney injury was defined according to a modified RIFLE criteria developed by the Acute Kidney Injury Network (AKIN). Differences among variables were evaluated by the Chi-square test and Mann-Whitney U test for categorical and continuous variables, respectively.
Results
Data from a total of 169 patients was collected. Only 119 developed fever, thus far 50 patients were excluded. Out of those 119 patients, 13 had fever outside the engraftment period, therefore a total of 106 patients were analyzed. From these, 50 (47.1%) received vancomycin and 56 (52.9%) did not. Eighteen patients (17%) out of the entire group had multiple myeloma and 88 (83%) lymphoma (Hodgkin and non-Hodgkin).
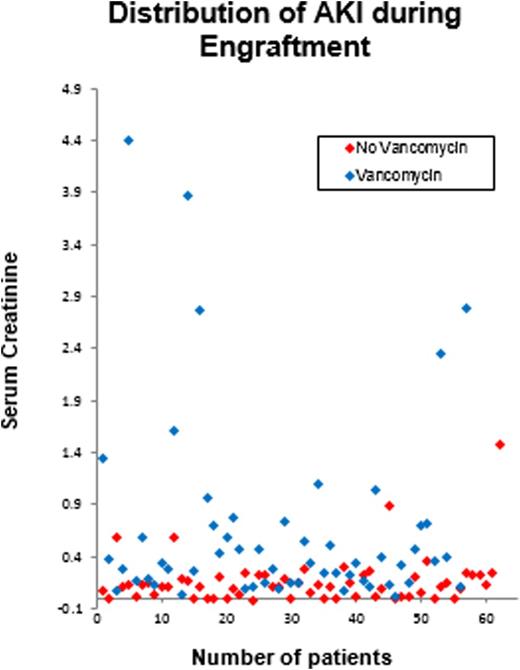
Twenty seven (54%) patients who received vancomycin had an abrupt (within 48 hours) absolute increase in the serum creatinine concentration of ≥0.3 mg/dL from baseline compared to the control group (p<0.05). From the same group, 20 (40%) patients experienced ≥50 percent increase in the serum creatinine and 2 patients (4%) required dialysis. In comparison, only 5 (8.9%) of the patients in the not vancomycin group developed AKI (p<0.05). (See figure 1).
Conclusion
Acute kidney injury related to treatment with vancomycin in patients who develop fever at the time of engraftment is a frequent complication in the studied population. Judicious use of vancomycin with close monitoring of renal function and fluid status during engraftment period is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.