Abstract
Introduction: The Charlson Comorbidity Index (CCI) has been adapted to claims-based analyses to assess comorbidity burden in cancer patients (primarily with solid tumors). We aimed to validate the CCI's prognostic significance in older lymphoma patients.
Methods: Using data from the Surveillance, Epidemiology, and End Results (SEER) Program linked with Medicare claims, we identified lymphoma patients 66 years and older using ICD-O codes from 1995-2010. We measured comorbidity burden in the year prior to patients' lymphoma diagnosis by calculating the Deyo/Klabunde-modified CCI scores using diagnosis codes in the claims (J Clin Epidemiol 2000). We estimated the unadjusted and adjusted association of CCI scores and demographic factors with overall survival (OS) and chemotherapy use at 6 months using a modified Poisson and logistic regression models.
Results: We identified 8,961 newly diagnosed patients with follicular lymphoma (FL), 19,997 diffuse large B-cell lymphoma (DLBCL), and 2,171 mantle cell lymphoma (MCL), of which 54%, 65%, and 63% received chemotherapy within 6 months of their cancer diagnoses, respectively. Age, gender, CCI, marital status, race, median income, and stage were significantly different between patients who received therapy and those who did not.
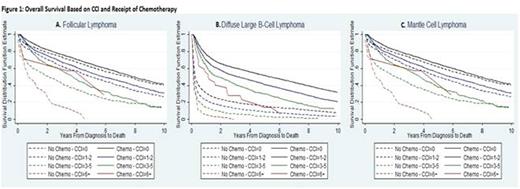
Average CCI was lower in those who were treated vs not [FL 0.76 vs 0.82 (p=0.06), DLBCL 0.84 vs 1.12 (p<0.001), and MCL 0.83 vs 1 (p=0.04)]. The CCI was predictive of 2 year-OS for FL, DLBCL, & MCL with a risk ratio of 0.91 (95%CI 0.89-0.93), 0.83 (0.8-0.86) and 0.89 (0.82-0.97) for CCI 1-2 vs 0; 0.72 (0.67-0.77), 0.58 (0.54- 0.62) and 0.68 (0.57-0.81) for CCI 3-5 vs 0; and 0.54 (0.34- 0.87), 0.37 (0.24-0.57) and 0.83 (0.45-1.55) for CCI 6+ vs 0, respectively (Figure 1A,B,C).
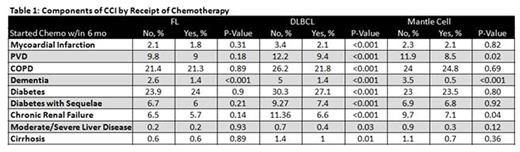
For all three subtypes, in addition to CCI, older age, female gender, living in a more rural area, race other than Caucasian, higher stage, and not receiving chemotherapy were also significantly associated with worse OS in the adjusted analysis. Within the CCI, the majority of the disease categories (myocardial infarction, peripheral vascular disease, chronic obstructive pulmonary disease, dementia, diabetes, diabetes with sequelae, chronic renal failure, moderate/severe liver disease, and cirrhosis) were more frequent in patients who did not receive treatment, particularly for DLBCL (Table 1). However, the overall predictive ability of our model for identifying patients who would receive chemotherapy was low (c-statistic =0.707).
Conclusion: In this first ever analysis of the CCI in lymphoma patients, we are able to confirm the utility of this scoring system in a new population. The majority of patients with three common lymphoma histologies captured in SEER-Medicare started treatment within 6 months of diagnosis. Comorbidity burden at diagnosis, measured by the Deyo/ Klabunde -modified CCI, is prognostic of OS for FL, DLBCL, and MCL. However, CCI along with other demographic non-clinical patient characteristics do not predict treatment initiation among older adults with lymphoma. Further claims analyses evaluating survival can include the CCI as an important variable.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.