Abstract
Background. Complement pathways are important targets for treatment of paroxysmal nocturnalhemoglobinuria (PNH) and autoimmune diseases. Because complement is essential in host defense against Neisseria, patients treated with complement inhibitors are at increased risk of life-threatening meningococcal disease. Meningococcal vaccination is recommended. However, the ability of vaccine-induced antibodies to confer protection when different complement pathways are blocked is poorly understood. Inhibiting formation of the membrane attack complex, C5b-C9, blocks serum bactericidal activity (SBA). In the absence of SBA, antibodies can prevent meningococcal disease byopsonophagocytosis (OPA) by binding of antibody to bacteria and activation of C4b and C3b via the classical pathway (CP). When antibody is limited, or the antigenic target is sparse, amplification of C3b deposition via the alternative pathway (AP) is required. OPA killing also depends on activation of phagocytic cells and up-regulation of Fc- and CR3 receptors, which is stimulated by C5a. In this study, we used a whole blood meningococcal killing assay to investigate blocking terminal pathway components C5 or C7 on bacterial survival. We also investigated the effect of blocking the AP using a small molecule factor D inhibitor.
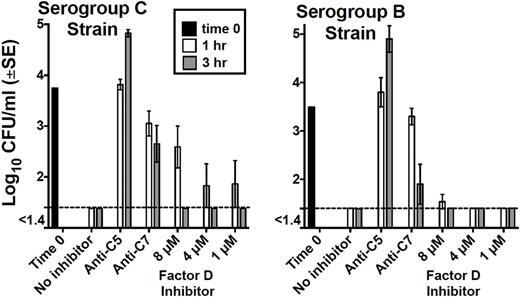
Methods. Bloodanticoagulated withlepirudin was obtained from five adults previously immunized with a meningococcal polysaccharide or conjugate vaccine. Four subjects also had completed serogroup B vaccination within 10 months. At time 0, ~5000cfu/ml of serogroup B or C bacteria were added to blood. Meningococcal killing was measured after incubation for 1 and 3hrs in the presence or absence of 50 µg/ml of anti-C5 (eculizumab) or a mouse anti-C7 mAb, both of which blocked SBA, or by 1 to 8 µM of a factor D inhibitor (ACH-4471,Achillion) that inhibited Factor D. By ELISA, 1 µM of the factor D inhibitor completely blocked the AP at 1 µM (the lowest concentration tested) and at 8 µM (the highest concentration tested) had no effect on CP.
Results. In the absence of inhibitor, blood from all five subjects incubated with bacteria showed no growth after 1 hr (<50 colony forming units (cfu)/mL). For the serogroup C strain, addition of the C5 inhibitor abolished bacterial killing, as evidenced by lack of decrease in cfu/mL at 1 hr relative to time 0, and an increase of >1 log10 cfu/mL at 3 hr (geometric mean, 74,200, Figure, left Panel). With the C7 inhibitor, cfu/mL decreased at 1 hr (p=0.04) and 3 hr (p=0.07) relative to time 0, and at both time points cfu/mL was significantly lower than with the anti-C5 inhibitor (p<0.007). In blood from four subjects tested, addition of the Factor D inhibitor had less effect on inhibiting serogroup C bacterial killing than anti-C5 or anti-C7 as evidence by an average of 1 log10 decreased cfu/mL at 1 hr with the Factor D inhibitor relative to time 0, and <50 cfu/mL at 3 hr. Similar results were obtained with the serogroup B strain by the addition of the C5 or C7 inhibitor to the blood from the three vaccinated subjects tested, and the addition of the Factor D inhibitor did not interfere with bacterial killing (<50 cfu/mL at 1 hr and 3 hr, Figure, right Panel). When tests were done with blood from a serogroup B unvaccinated subject, the Factor D inhibitor blocked killing (42,000 cfu/mL at 3 hr). In experiments with blood from two vaccinated subjects and serogroup B and C strains, the addition of a C5a receptor antagonist to blood containing anti-C7 increased cfu/mL by >1 log10 at 3 hr, compared to anti-C7 alone.
Conclusions. Blocking C5 cleavage and release of C5a by a C5 inhibitor impairs both SBA and OPA killing of meningococci in whole blood, which provides a biologic basis for reports of failure of vaccination in preventing meningococcal disease in some patients treated witheculizumab. Blocking C7 impairs SBA but has less effect on impairing whole blood OPA killing than with anti-C5, since release of C5a, which stimulates phagocytic cell activity, is not inhibited by anti-C7. Effective killing of meningococci by blood from vaccinated subjects was seen at 3 hr (< 50cfu/mL) in the presence of ACH-4471. However, ACH-4471 impaired killing of serogroup B strain by blood from an unvaccinated adult, in which bacterial killing depended on the AP. These data suggest that vaccination may be more effective in decreasing the risk of meningococcal disease in the presence of an AP inhibitor as compared to a C5 inhibitor.
Granoff:Achillion Pharmaceuticals: Other: Consultant, ended May 1, 2016, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.