Abstract
There is a high prevalence of obstructive sleep apnea (OSA) in the United States, with one-quarter of adults aged 30 to 70 years having OSA. Most clinicians consider OSA as one of the causes of elevated hemoglobin (Hb) - polycythemia, but this is based on anecdotal evidence and further work up is often not pursued. Chronic intermittent hypoxia associated with OSA can augment hypoxia-inducible factor-2, the principal regulator of erythropoietin, and may increase red cell mass. But there is a paucity of published data evaluating the effects of OSA and treatment with continuous positive airway pressure (CPAP) on hematologic parameters.
We conducted a retrospective analysis of 5152 patients evaluated for OSA with polysomnography at the University of Utah Sleep-Wake Center from January 2013 to October 2015. Hematologic, other laboratory and clinical parameters were available for 527 patients prior to and after therapy of OSA with CPAP. OSA severity was defined as mild (apnea hypopnea index (AHI) 5-15 events/hr), moderate (AHI 15-30/hr) or severe (AHI >30/hr). Data on AHI, lowest oxygen saturation (SpO2) and time spent at SpO2 < 89% were obtained from polysomnography. Other evaluated parameters were age, gender, body mass index, CBC prior to starting CPAP; and Hb and hematocrit (Hct) at 3, 6, 12 and 18 month time points during CPAP therapy. Information regarding comorbidities and medication use that could influence red cell mass was also collected. WHO criteria were used to define polycythemia as Hb >18.5 and 16.5 gm/dl in males and females, respectively.
This study included 527 patients, 254 females (48.19%) and 273 males (51.8%), who had at least one Hb measurement prior to starting CPAP therapy. Twenty-one (4%) out of 527 patients had polycythemia, of which 12 were on testosterone supplementation or used home oxygen for chronic pulmonary disease. Excluding these 12 patients resulted in a lower prevalence of polycythemia in OSA of 1.7% (9 patients).
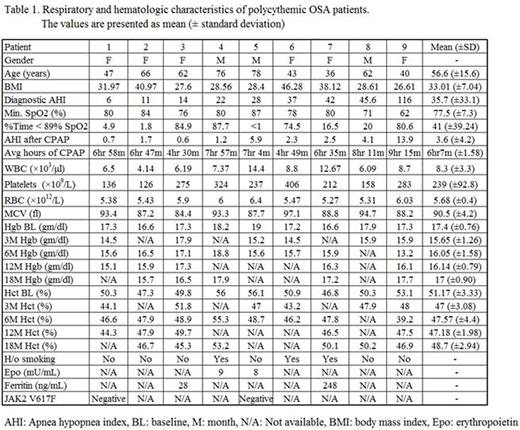
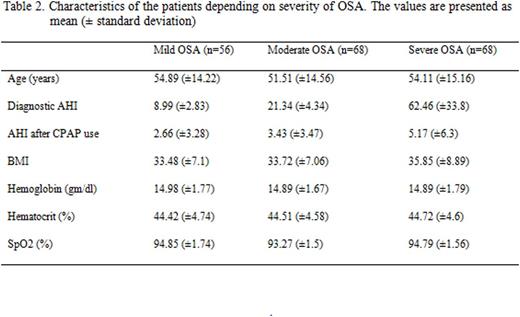
JAK2 mutational status or erythropoietin levels, however, were not available for all patients. The polycythemic cohort included 6 females and 3 males with a mean age of 56.6 years. The mean AHI was 35.7; 3 patients had mild, 2 moderate, and 4 severe OSA. Common comorbidities included hypertension (n=5), stroke (n=2) and diabetes (n=2). The mean Hb before CPAP therapy was 17.4 gm/dl, which corrected to normal during CPAP usage in 7 but not in 2. In these 2 patients, Hb corrected to normal with CPAP usage, but increased again by 18 months despite continued CPAP use. The mean Hb was lowest after 3 months of CPAP use and gradually increased thereafter (Table 1). Analysis of mean Hb concentration between different OSA severities (mild, moderate and severe) did not show any significant difference (Table 2).
However, when analysis was performed using the normal range for the laboratory used, an additional 16 (3%) patients had Hb above the upper limit of normal (15.9 gm/dl for females and 17.8 gm/dl for males). This resulted in a 7% prevalence of polycythemia in OSA. Excluding patients on testosterone or with chronic lung disease, the overall prevalence was 4.5% (24 patients). Seventeen (3.2%) patients had elevated Hct with normal Hb.
Here we report the results from a large dataset of OSA patients measuring the prevalence of polycythemia. Our results show that polycythemia is rarely seen in OSA patients, and other potential causes of polycythemia should be evaluated before attributing it to OSA. The degree of OSA severity does not seem to correlate with Hb level. In those rare polycythemic OSA patients, polycythemia is corrected by CPAP therapy in the majority. However, with the revised WHO criteria for diagnosis of polycythemia vera (16 and 16.5 gm/dl for females and males, respectively), we anticipate that more patients with OSA will be considered to have polycythemia.
The low prevalence of polycythemia may be attributed to neocytolysis, wherein transition from sustained hypoxia to normoxia leads to overcorrection of polycythemia due to transient expansion of mitochondria-generating reactive oxygen species, with preferential destruction of young red cells made in hypoxia (Song et al, Mol Med, 2015). We are currently investigating whether neocytolysis also occurs in OSA, which however is characterized by chronic, rapid, repetitious cycles of hypoxia and normoxia that may preclude development of polycythemia in a majority of patients.
First and second authors listed contributed equally.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.