Abstract
Background. Immune thrombocytopenia (ITP) is an autoimmune bleeding disorder that results in thrombocytopenia and the risk of bleeding. Severe bleeding, while uncommon, is partially associated with the degree of thrombocytopenia. However it remains unclear why some thrombocytopenic patients with ITP have significant bleeding while others have minimal or no bleeding manifestations. We hypothesized that differences in platelet function between ITP patients contribute to the variation in bleeding tendency and these differences can be used to identify children at the highest risk for bleeding. We recently reported (Frelinger et al. Blood 2015;126:873-879) that platelet tests related to platelet age (immature platelet fraction [IPF], forward light scatter [FSC]) and activation through the PAR1 thrombin receptor (TRAP-stimulated P-selectin, activated GPIIb-IIIa, and GPIba) are associated with concurrent bleeding severity in ITP, independent of the platelet count.
Aims. 1) Determine the association of platelet function tests with subsequent bleeding severity. 2) Determine the consistency of the platelet function phenotype over time.
Methods. At two study visits separated by at least 1 month, bleeding severity (graded by the Buchanan and Adix Score) and platelet function tests were evaluated in a single center cross-sectional study of patients ≥6 months of age with a diagnosis of ITP or Evans syndrome. Platelet function was assessed by whole blood flow cytometric analysis of platelet surface P-selectin, activated GPIIb-IIIa (measured by monoclonal antibody PAC1), and GPIbα with and without in vitro agonist (ADP or thrombin receptor activating peptide [TRAP]) stimulation. Complete blood cell counts, including IPF, were obtained in a Sysmex XN-1000.
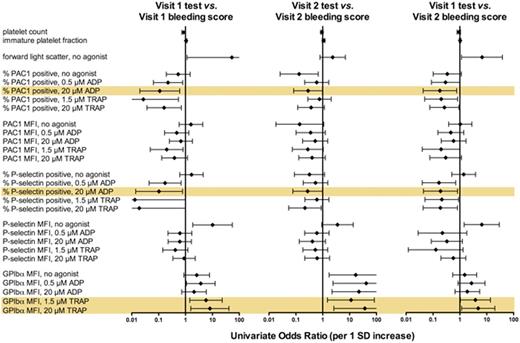
Results. Fifteen patients (9.5 ± 5.2 [mean ± SD] years of age, 4 male) were evaluated with a median interval between visits of 10.1 months (interquartile range 2.3 - 23.9 months). Bleeding severity was lower at Visit 2 compared to Visit 1 (Visit 1: Grade 0, n=4, Grade 1, n=4, Grade 2, n=6, Grade 3, n=1 vs. Visit 2: Grade 0, n=7, Grade 1, n=6, Grade 2, n=1, Grade 3, n=1, p = 0.0107). At Visit 2 mean platelet count was higher and IPF was lower than at Visit 1 (111 vs. 69 x 109 platelets/L, p = 0.06 and 10.7 vs. 14.3% IPF, p = 0.04). Nevertheless, platelet count and IPF at Visit 1 were both strongly correlated with platelet count and IPF, respectively, at Visit 2. At each visit, % P-selectin-positive platelets with 20 µM ADP, % PAC1-positive with 20 µM ADP, and GPIba mean fluorescence with 1.5 and 20 µM TRAP, were associated by univariate analysis with the concurrent bleeding score (Figure). Platelet function in patients with ITP was consistent over time as demonstrated by: a) significant correlations between platelet count, IPF, and circulating or agonist-stimulated platelet surface P-selectin, activated GPIIb-IIIa, and GPIba at Visit 1 vs. Visit 2; b) significant associations between platelet markers at each visit with bleeding scores at each visit; and c) a significant association of platelet markers at Visit 1 with bleeding scores at Visit 2 (Figure).
Conclusions. Platelet function tests identify a platelet phenotype in children with ITP that is consistent over time and is associated with bleeding severity at both concurrent and subsequent visits. These results suggest the platelet phenotype contributes to the bleeding risk in children with ITP and supports further evaluation of platelet function testing to help guide patient management.
Univariate association of platelet tests with bleeding score at concurrent and subsequent visits. Tests significantly associated with bleeding score in all comparisons are highlighted.
Univariate association of platelet tests with bleeding score at concurrent and subsequent visits. Tests significantly associated with bleeding score in all comparisons are highlighted.
Frelinger:Sysmex: Research Funding. Grace:Agios Pharmaceuticals: Other: Scientific Advisor, Research Funding. Michelson:Sysmex: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.