Abstract
INTRODUCTION: Over the last years multiparameter flow cytometry (MFC) has proven an effective method for the detection of minimal residual disease (MRD) not only in Acute Lymphoblastic Leukemia but also in Acute Myeloid Leukemia (AML) (Inaba, JCO 2012) providing powerful independent prognostic information (Loken, Blood 2012; Freeman, JCO 2013) in addition to molecularly-based approaches. It is unclear if it should be useful in all AML patients (pts) with a detectable leukemia associated immune-phenotype (LAIP) or just in pts without a molecular marker. Herein we report the results obtained in a consecutive series of pts followed at our institution.
METHODS: Between July 2010 and March 2016, we analyzed MRD by MFC in 144 AML pts treated according to NILG AML study (Bassan, Blood 2003) at diagnosis and at the following subsequent time points (TP): achievement of complete remission (CR) after 1 or 2 courses of induction therapy (TP1), after the first consolidation course (TP2) and at the end of the treatment program (TP3). Bone marrow samples were analyzed by eight/six-colours MFC, the cut-off value used for MRD was 0.1% and 0.035% at TP1 (Al-Mawali, 2009) and 0.035% at TP2 and TP3 (Buccisano, Blood 2010). Molecularly based real-time quantitative PCR (RT-PCR) methods were used to monitor CBF in 10 pts and NPM1 in 25 pts (Gorello, Leukemia 2006). The pts median age was 56 years (19-73y), the F/M 59/85; de-novo AML 125/144 (86.8%) and secondary AML (s-AML) were 19/144 (13.2%). Most pts belonged to the intermediate (int) cytogenetic risk group (MRC favorable n=12, 8.3%, int n=105, 73%, adverse n=27, 18.7%), while the distribution according to ELN risk group was 51 favorable (35.4%), 47 int-I (32.6%), 19 int-II (13.2%) and 27 adverse (18.8%), respectively.
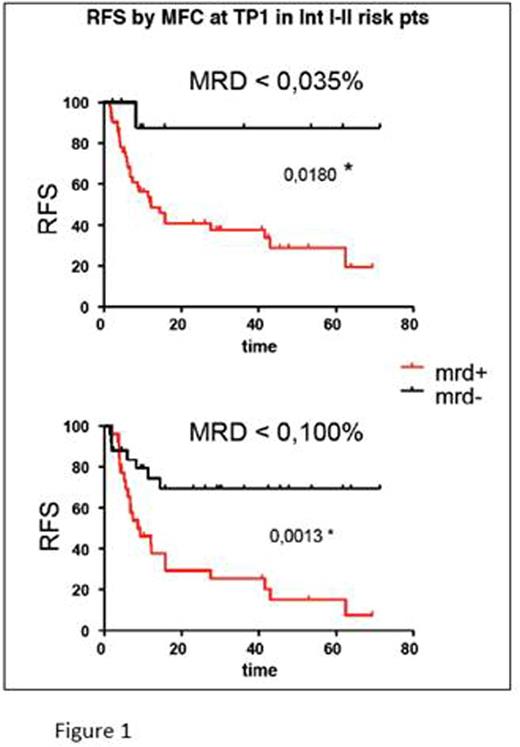
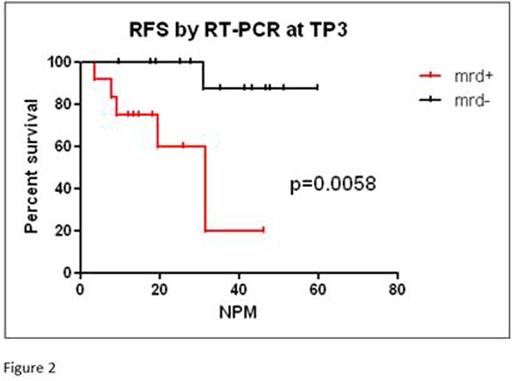
RESULTS: At diagnosis 120/144 pts (83.3%) had a LAIP. There were no differences in clinical or biologic characteristics between pts with or without a LAIP, except that in the no-LAIP group the s-AML and adverse risk ELN were more represented (25% vs 10.7% and 25% vs 16.6%, respectively). In pts with LAIP, after a median follow-up of 23 months (ms), the CR rate was 88.3%, median relapse free survival (RFS) was 49%+/-7 ES, at 5y and median overall survival (OS) was 57.9 ms, with no differences compared to no-LAIP pts. Distribution among cytogenetic and molecular risk groups was as follows: for MRC favorable n=10 (8.3%), int n=90 (75%), adverse n=20 (16.7%); according to ELN risk: 43 favorable (35.8%), 40 int-I (33.3%), 17 int-II (14.2%), and 20 adverse (16.7%). The ELN risk classification stratified both for OS (p=0.004) and for RFS (p=0.0095), while MRC classification did not (p=0.33 and p=0.36, respectively). In the LAIP group we serially analyzed marrow cells at the different TP: 106/120 at TP1 (10 pts did not reach CR, 4 inadequate sample), 99 at TP2, while 66 were evaluable at TP3. MRD negativity was achieved at TP1 in 52/106 (49%) and in 21/106 (19.8%) pts with a threshold of 0.1% and 0.035%, respectively; at TP2 in 35/99 (35.4%) and at TP3 in 19/66 (24.2%). According to risk classification, at TP1 MRD positivity by MFC predicted relapse in int-I and int-II ELN risk groups, both with a threshold of 0.035% (p=0.018), and of 0.1% (p=0.0013) (Figure 1). The median of time to relapse was 11.9 ms in MRD positivity and 14.4 ms in MRD negativity pts. In the other ELN risk group there was no difference in relapse rate according to MRD negativity (p=0.19 and p=0.9 in favorable and p=0.16 and p=0.7 in adverse, respectively, according to 2 threshold). In the favorable ELN group the comparison of MRD results obtained by MFC with those obtained by RT-PCR was possible in 25 pts with NPM-mutated AML who achieved CR in 100% and relapsed in 20% of cases. MRD by MFC resulted detectable in 2 pts (8%) at TP1, in 7 pts at TP2 (28%), and in 13 of 25 pts (53%) at TP3, with no correlation with relapse risk. MRD positivity by RT-PCR predicted the relapse at TP2 (p=0.07) and at TP3 (p=0.0058) (Figure 2).
CONCLUSION: Methods for determining MRD in AML may differ in their accuracy. Our study confirms that while in pts with favorable ELN risk AML, molecular methods may be considered the gold standard, in pts without a molecularly evaluable marker, the use of MFC may be useful for predicting relapse. Promising results of MFC MRD determination were achieved in the subset of AML at ELN intermediate risk where it is clinically most helpful in supporting the difficult choice among different postremission treatment strategy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.