Abstract
Background: Duvelisib is an oral, dual inhibitor of PI3K-d,γ, in development for the treatment of hematologic malignancies, including follicular lymphoma (FL). Duvelisib disrupts PI3K-d,γ-mediated signaling within tumor cells and their interactions with the tumor microenvironment, hindering hematologic tumor cell survival. Data from a Phase 1 study of duvelisib indicate the potential for duvelisib to be an effective treatment for FL, with an acceptable safety profile. CONTEMPO (NCT02391545), is designed to evaluate the safety and clinical activity of duvelisib in combination with rituximab (DR) or obinutuzumab (DO) in patients (pts) with previously-untreated CD20+ FL.
Methods: In CONTEMPO, duvelisib is administered at 25 mg BID continuously in 28-day treatment cycles, combined either with rituximab (375 mg/m2 for 4 weekly doses, then 1 dose every 2 cycles) or obinutuzumab (1000 mg for 4 weekly doses, then 1 dose every 2 cycles). Pts are assigned 1:1 into the two parallel treatment arms. Key inclusion criteria include: diagnosis of previously-untreated CD20+ FL, Stage II with bulky disease (≥ 7 cm lesion), or Stage III-IV disease, at least 1 measurable disease lesion > 1.5 cm, adequate liver and renal function, and no clinical evidence of transformation to a more aggressive subtype of lymphoma or Grade 3B FL. Prophylaxis for herpes (HSV/VZV) is recommended. For pts with a history of CMV infection requiring treatment, prophylaxis and monitoring of reactivation is recommended. The original protocol mandated PJP prophylaxis when CD4 counts were ≤ 200 cells/mm3, and was subsequently amended to include all pts. Disease response assessments (CT scans and physical exams) occur on Day 1 of Cycle 4 (C4), C8, C12, C16, C20, and C26.
Results: As of 19 July 2016 (data cut-off), 28 pts received DR and 27 received DO. For DR pts, the median age was 58 years, most were male (64%), 21% had Gr 1 and 64% Gr 2 disease at baseline, and 54% had bone marrow involvement. Median time from diagnosis was 2.3 months. For DO pts, the median age was 58 years, most were female (59%), 48% had Gr 1 and 30% Gr 2 disease at baseline, and 59% had bone marrow involvement. Median time from diagnosis was 2.6 months. DR pts were on treatment for a median of 3.9 months, DO pts for 4.5 months.
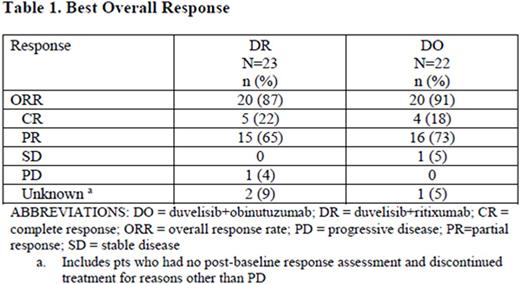
The overall response rate (ORR) per IWG criteria for DR was 87% and for DO was 91% (see table)
The rate of AEs for DR pts was 93%, with 50% having a ≥ Gr 3 AE. 64% of DR pts had an AE leading to duvelisib dose modification (reduction or hold), while 14% discontinued duvelisib due to an AE. The most common ≥ Gr 3 AEs on DR (> 2 pts) were ALT increased (21%) and rash (14%). The rate of ≥ Gr 3 infections was 11%, including PJP (n=2; no prophylaxis, pre-amendment), followed by lung infection and pneumococcal pneumonia (1 pt, each). One PJP case resolved and the pt continued on study. The second PJP case resolved, however the pt had a subsequent fatal event of acute respiratory distress, the only fatal AE on study.
The rate of AEs for DO pts was 89%, with 70% of pts having a ≥ Gr 3 AE. 63% of DO pts had an AE leading to duvelisib dose modification (reduction or hold), while 7% discontinued duvelisib due to an AE. Most common ≥ Gr 3 AEs (> 2pts) on DO were neutropenia (19%), ALT increased (15%), and AST increased (11%). The rate of ≥ Gr 3 infections was 15%, including conjunctivitis, RSV pneumonia, pyelonephritis, and septic shock (1 pt, each). No pts on DO died due to an AE.
Conclusions: Preliminary clinical activity with DR (87% ORR, 22% CR) and DO (91% ORR, 18% CR) supports the potential role of duvelisib in combination with an anti-CD20 monoclonal antibody as initial treatment for pts with FL. The safety profile was manageable with appropriate risk mitigation measures, suggesting further investigation of these combinations may be warranted.
Casulo:Celgene: Research Funding; Infinity: Consultancy, Honoraria. Sancho:Gilead: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Celltrion, Inc: Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Gyan:Amgen: Honoraria; Sanofi: Honoraria; Pierre Fabre: Honoraria; Novartis: Research Funding; Celgene: Research Funding; Fresenius Kabi: Honoraria; Gilead: Consultancy, Speakers Bureau; Mundipharma: Consultancy; Roche: Research Funding. Steelman:Infinity: Employment. Pearlberg:Infinity: Employment. Goy:Genentech: Research Funding; Johnson & Johnson: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Acerta: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Pharmacyclics LLC, an AbbVie Company: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; infinity: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Other: Writing support, Speakers Bureau; Celgene: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.