Abstract

Background:The Janus kinase (JAK) 1/JAK2 inhibitor ruxolitinib has been evaluated for patients with MF in the phase 3 COMFORT studies. In both trials, ruxolitinib prolonged OS, reduced splenomegaly, and improved MF-related symptoms and quality of life compared with controls. Here, we report the results of an exploratory pooled analysis of OS in the COMFORT studies at 5 years of follow-up.
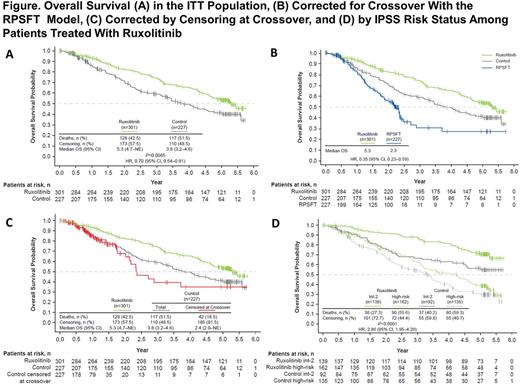
Methods: The double-blind COMFORT-I trial and the open-label COMFORT-II trial were randomized phase 3 studies that evaluated the safety and efficacy of ruxolitinib in patients with intermediate-2 (int-2) or high-risk primary MF (PMF), post-polycythemia vera MF (PPV-MF), or post-essential thrombocythemia MF (PET-MF). The comparator was placebo in COMFORT-I and best available therapy (BAT) in COMFORT-II. The ruxolitinib starting dose was 15 or 20 mg twice daily based on baseline platelet counts (100-200 and >200 × 109/L, respectively); dose modifications were permitted for safety and efficacy. Patients were allowed to cross over to ruxolitinib from the control arm for progressive splenomegaly, defined as a ≥25% increase in spleen volume from baseline (COMFORT-I) or study nadir (COMFORT-II), or select protocol-defined progression events; crossover was mandatory following treatment unblinding in COMFORT-I. OS was a secondary endpoint in both studies and was evaluated in an intent-to-treat (ITT) analysis using a Cox proportional hazard model that estimated the treatment effect stratified by clinical trial and International Prognostic Scoring System (IPSS) risk. The crossover-corrected treatment effect was estimated using a rank-preserving structural failure time (RPSFT) method.
Results: Overall, 528 patients were randomized: 301 to ruxolitinib (COMFORT-I, n=155; COMFORT-II, n=146) and 227 to placebo (n=154) or BAT (n=73). All ongoing patients in the control arms crossed over to ruxolitinib by the 3-year follow-up. Patient populations were similar between the two trials and their details were previously published. In the combined ruxolitinib group, 162 patients (53.8%) had high-risk MF and 139 (46.2%) had int-2 risk MF based on IPSS criteria. At the 5-year ITT analysis, 128 patients (42.5%) died in the ruxolitinib group compared with 117 (51.5%) in the control group. The risk of death was reduced by 30% with ruxolitinib compared with control (median OS: ruxolitinib, 63.5 mo; control, 45.9 mo; HR, 0.70; 95% CI, 0.54-0.91; P=0.0065; Figure A). After correcting for crossover using RPSFT, OS advantage was more pronounced for patients originally randomized to ruxolitinib (median OS: ruxolitinib, 63.5 mo; control, 27 mo; HR, 0.35; 95% CI, 0.23-0.59; Figure B). An analysis of OS censoring patients at the time of crossover also demonstrated that ruxolitinib prolonged survival compared with control (median OS: ruxolitinib, 63.5 mo; control, 28.3 mo; HR, 0.53; 95% CI, 0.36−0.78; P=0.0013; Figure C). Among all patients treated with ruxolitinib, those with lower-risk disease had longer survival compared with those with high-risk disease (median OS: int-2, not reached [estimated, 102 mo]; high-risk, 50 mo; HR, 2.86; 95% CI, 1.95-4.20; P<0.0001; Figure D). In a subgroup analysis, OS favored ruxolitinib compared with placebo for patients with int-2 or high-risk MF (data not shown). At 5 years, median OS appeared to favor patients with int-2 (n=58) or high-risk (n=89) PMF who were originally randomized to ruxolitinib compared with historical (Cervantes et al; J Clin Oncol 30:2981-2987) controls (int-2 PMF, not reached [estimated, 70 mo] vs 48 mo; high-risk PMF, 34 vs 27 mo); OS was longer among patients with int-2 vs high-risk PMF (P=0.0003). Subgroup analyses showed that ruxolitinib provided an OS advantage regardless of age (>65 or ≤65 y), sex, disease type (PMF, PPV-MF, PET-MF), risk status (int-2 or high), JAK2V617F mutation status, baseline spleen volume (>10 or ≤10 cm), anemia, white blood cell count (>25 or ≤25 × 109L), or platelet count (>200 or ≤200 × 109/L).
Conclusion: Long-term treatment with ruxolitinib up to 5 years prolonged survival in patients with MF compared with BAT or placebo. Corrections for patients who crossed over to ruxolitinib suggested that the separation between ruxolitinib and control OS curves was primarily caused by a delay in ruxolitinib treatment. The results suggest that earlier treatment with ruxolitinib may provide a greater survival advantage for patients with MF.
Gupta:Incyte Corporation: Consultancy, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Mesa:Incyte: Research Funding; Ariad: Consultancy; Novartis: Consultancy; Celgene: Research Funding; CTI: Research Funding; Promedior: Research Funding; Galena: Consultancy; Gilead: Research Funding. Vannucchi:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Kiladjian:AOP Orphan: Research Funding; Novartis: Research Funding. Cervantes:AOP Orphan: Membership on an entity's Board of Directors or advisory committees; Baxalta: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Sun:Incyte Corporation: Employment, Equity Ownership. Gao:Incyte Corporation: Employment, Equity Ownership. Dong:Novartis Pharmaceutical Corporation: Employment, Equity Ownership. Naim:Incyte Corporation: Employment, Equity Ownership. Gopalakrishna:Novartis Pharma AG: Employment, Equity Ownership. Harrison:Incyte Corporation: Honoraria, Speakers Bureau; Baxaltra: Consultancy, Honoraria, Speakers Bureau; Gilead: Honoraria, Speakers Bureau; CTI Biopharma: Consultancy, Honoraria, Speakers Bureau; Shire: Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Other: travel, accommodations, expenses, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract