Abstract
Introduction: Entospletinib is an orally bioavailable, selective inhibitor of spleen tyrosine kinase. Targeting the B-cell receptor (BCR) signaling pathway with Bruton's tyrosine kinase (BTK) and PI3Kd inhibitors (BTKi and PI3Kdi), approved for treatment of chronic lymphocytic leukemia (CLL), has been a successful therapeutic strategy. Entospletinib is active in CLL and preclinical data suggest that entospletinib may be effective even in the context of resistance to BTKi, including that conferred by activation of PLCγ2 (Liu et. al. Blood 2015).
Methods: This is an ongoing phase 2 trial (NCT01799889) of entospletinib in CLL and non-Hodgkin lymphoma. The study protocol includes 2 CLL cohorts for patients who have been previously treated with BTKi or PI3Kdi and 2 additional cohorts for patients with Richter's transformation who have had analogous prior treatment. Patients were treated with entospletinib monotherapy (400 mg BID) and evaluated using modified Hallek/IWG-CLL criteria every 2 to 3 months as previously described (Sharman et. al. Blood 2014).
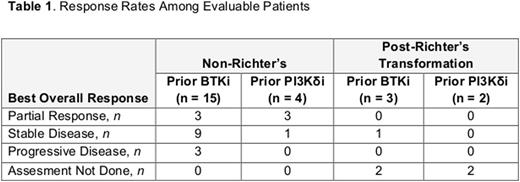
Results: As of June 28, 2016, 34 patients have been enrolled, and 33 have been treated. Of the 28 patients without Richter's transformation, 23 were previously treated with a BTKi (22 ibrutinib, 1 CC-292) and 5 with a PI3Kdi (idelalisib). Median number of prior treatments was 3 (1-7) for patients with prior BTKi and 5 (3-8) for prior PI3Kdi treatment. In total, 35% of the BTKi patients and 60% of the PI3Kdi patients had either a TP53 mutation or del17p; 75% did not have IgHV hypermutation. A median of 2 months (0-14) had elapsed since the prior treatment; 17 patients had progressive disease on prior therapy, while 11 discontinued prior therapy due to intolerance. Thirteen of the 28 patients enrolled without Richter's transformation remain on study with a median PFS of 5.6 months for the prior BTKi cohort and a median PFS of 6.9 months for the prior PI3Kdi cohort. Of the 15 patients who have stopped therapy, 9 discontinued due to disease progression, 5 discontinued due to an AE, and 1 withdrew consent. Overall, 19 patients were evaluable for response (15 BTKi/4 PI3Kdi; Table 1). Of the 6 patients who achieved a PR, all lacked IgHV hypermutation and 3 had either a TP53 mutation or del17p, and 3 had progressed on prior therapy. Following Richter's transformation, 5 patients have been treated with entospletinib (3 with prior BTKi therapy and 2 with prior PI3Ki). The interval since prior treatment was short (<1 month in 4/5 with 1 missing) with 3 to 6 prior lines of treatment. One patient with prior BTKi therapy and Richter's transformation remains on study with 118 days on treatment; 4 patients discontinued treatment due to progressive disease (at 40 and 67 days following prior BTKi and 8 and 28 days following prior PI3Kdi).
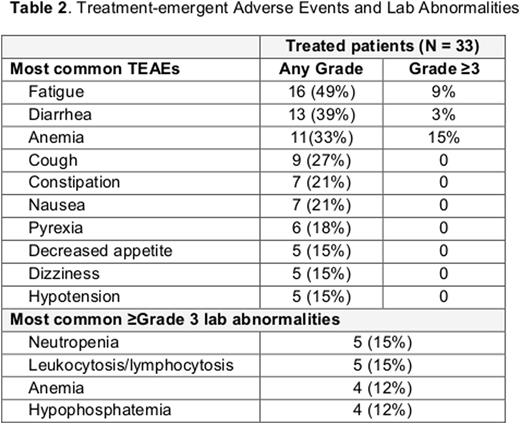
All patients on study experienced a treatment-emergent AE (TEAE) and 49% experienced a serious AE (SAE; Table 2). Only 1 SAE, pancreatitis, was attributed to entospletinib. The most common TEAEs and laboratory abnormalities are listed in Table 2. Additional Grade ≥3 TEAEs reported in more than 1 patient included sepsis (3), atrial fibrillation (2), dehydration (2), neutropenia (2), pneumonia (2), respiratory failure (2), and urinary tract infection (2). The only TEAE attributable to entospletinib that led to discontinuation of treatment was fatigue. Five patients died on study; 2 from progressive disease and 1 each from heart failure, Guillain-Barre syndrome, and cardiac arrest; 3 of these 5 patients died within 30 days of the last dose of study drug [disease progression (2), cardiac arrest (1)].
Conclusion: Early experience from this trial with ongoing enrollment demonstrates that entospletinib has clinical activity following therapy with either BTKi or PI3Kdi. Continued investigation of treatment with entospletinib following progression after therapy with BCR signaling pathway inhibitors is warranted.
Sharman:Gilead Sciences, Inc.: Honoraria, Research Funding. Shustov:Celgene: Consultancy, Honoraria; SPECTRUM: Consultancy, Research Funding; Seattle Genetics: Research Funding; Novartis: Research Funding; BMS: Consultancy, Honoraria. Smith:Celgene: Honoraria; Spectrum: Honoraria; Abbvie: Research Funding; Genentech: Honoraria. Kolibaba:Cell Therapeutics: Research Funding; Gilead: Consultancy, Research Funding; Genentech: Research Funding; GSK: Research Funding; Janssen: Research Funding; Acerta: Research Funding; Amgen: Research Funding; Celgene: Research Funding; Novartis: Research Funding; Pharmcyclics: Research Funding; Seattle Genetics: Research Funding; TG Therapeutics: Honoraria, Research Funding. Abella-Dominicis:Gilead Sciences: Employment, Equity Ownership. Zhang:Gilead Sciences: Employment, Equity Ownership. Mitra:Gilead Sciences: Employment, Equity Ownership. Yasenchak:Seattle Genetics: Research Funding. Awan:Pharmacyclics: Consultancy; Innate Pharma: Research Funding; Novartis Oncology: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.