Abstract

Background: Cytogenetic evaluation using fluorescence in situ hybridization (FISH) at the time of diagnosis is essential for initial risk stratification in multiple myeloma. Despite the absence of cytogenetic high-risk abnormalities a subset of patients does experience poor overall survival comparable high-risk disease (i.e. median overall survival less than three years after diagnosis). We aimed to identify demographic, clinical, and cytogenetic characteristics predicting poor three-year overall survival in patients with standard-risk cytogenetics.
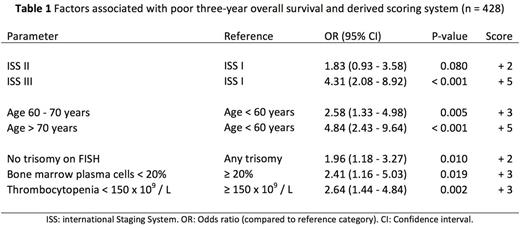
Methods: We studied 428 patients who were diagnosed with multiple myeloma between July 2004 and July 2014 at Mayo Clinic Rochester, underwent FISH evaluation within six months of diagnosis, and received treatment with novel agents (immunomodulator, proteasome-inhibitor, or a combination thereof). Patients with high- and intermediate-risk cytogenetics as well as patients lost to follow-up within three years were excluded. High-risk cytogenetics were defined as del(17p), t(14;16), and t(14;20). Intermediate-risk cytogenetics were defined as t(4;14) and gain(1q). Bone marrow aspirates were evaluated for deletions, monosomies, trisomies, and tetrasomies using chromosome- or centromere-specific FISH probes. IGH rearrangements were evaluated using an IGH break-apart probe and evaluating up to five potential partners (FGFR3, CCND1, CCND3, MAF, and MAFB). A multivariable-adjusted logistic regression model was used to assess the associations between the parameters of interest and three-year overall survival. Discrimination and calibration of the model were evaluated using the c-statistic and the Hosmer-Lemeshow test, respectively. The odds ratios of the identified predictors were rounded up to the next integer and assigned as points in a scoring system. Receiver operating characteristic analysis was used to determine the optimal cut-point and associated test performance characteristics. P-values below 0.05 were considered statistically significant.
Results: The median age at diagnosis was 65 years (31 - 95), 259 (61%) of the patients were male. The median overall survival was 7.4 years (6.1 - 8.6) for the entire cohort (n = 428), 10.5 years (8.3 - NR) for those who survived at least three years (n = 327, 76%), and 1.6 years (1.2 - 1.7) for those who did not survive three years after diagnosis (n = 101, 24%). The factors associated with poor three-year overall survival and the derived scoring system are summarized in Table 1.
Conclusions: Patients with multiple myeloma and standard-risk cytogenetics are a heterogeneous group. One fourth of the patients are experiencing less than three years of overall survival after diagnosis. Stage, age, extent of bone marrow involvement, karyotype, and platelet count at the time of diagnosis were helpful in identifying patients at risk for poor three-year overall survival. These findings emphasize the importance of further risk stratification in this patient population and warrant external validation.
Dispenzieri:Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Jannsen: Research Funding; pfizer: Research Funding; Prothena: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees; Celgene: Research Funding; Alnylam: Research Funding. Kapoor:Takeda: Research Funding; Amgen: Research Funding; Celgene: Research Funding. Kumar:AbbVie: Research Funding; BMS: Consultancy; Amgen: Consultancy, Research Funding; Takeda: Consultancy, Research Funding; Sanofi: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Noxxon: Consultancy, Honoraria; Janssen: Research Funding; Skyline: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract