Abstract
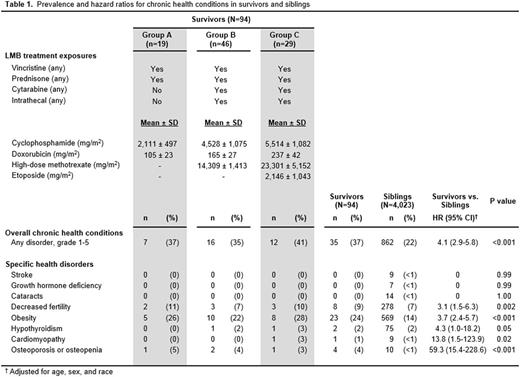
Introduction: Since the mid-1990's, overall survival rates for children diagnosed with mature B-cell non-Hodgkin lymphoma (B-NHL) have exceeded 90%, due in large part to the widespread utilization of the LMB chemotherapy regimen. As a result, a population of survivors living beyond 5 years from diagnosis and treatment with this regimen is emerging, providing the first opportunity to study late-occurring and chronic health outcomes following contemporary B-NHL therapy. Methods: Late health outcomes and health status were self-reported among CCSS participants who were 5-year survivors of childhood B-NHL and whose treatment exposures were consistent with LMB-defined risk-groups (A - low; B - intermediate; and C - high risk). Combinations of individual chemotherapy agents (cyclophosphamide [CPM], vincristine, prednisone, doxorubicin [doxo], high-dose methotrexate [HD-MTX], cytarabine, and etoposide) and respective cumulative doses (for CPM, doxo, HD-MTX, and etoposide) were abstracted from medical records. Chronic health conditions occurring ≥5 years from cancer diagnosis were graded per the Common Terminology Criteria for Adverse Events (version 4.03). Decreased fertility was defined as failure to achieve or sire a pregnancy after ≥1 year of trying among survivors of childbearing age (15-44 years). Health status outcomes were obtained from validated questionnaires. Standardized mortality ratios (SMRs) were estimated. Cox and logistic regression models (adjusted for age, sex, and race) provided hazard (HR) and odds ratios (OR) and 95% confidence intervals (CI) of health conditions and status compared to a sibling comparison group (n=4,023). Results: We identified 94 B-NHL survivors (median age 10 [range 2-20] years at diagnosis, 24 [10-39] years at evaluation, 14 [7-26] years post diagnosis), for which pertinent LMB treatment exposures are included in Table 1. Compared to siblings, survivors were more likely to be male (79% vs. 48%, p<0.001), younger at evaluation (24.3 ± 6.1 vs. 26.7 ± 9.2 years, p<0.001), and non-white race (22% vs 13%, p=0.006). Thirty-five (37%) survivors had ≥1 chronic condition (grades 1-5); a 4-fold increased risk (HR 4.1, 95% CI: 2.9-5.8) compared to siblings (Group A HR 2.6, 95% CI 1.2-5.6, Group B HR 5.2, 95% CI 3.1-8.6, and Group C HR 4.2, 95% CI 2.4-7.6). The most frequently occurring conditions were obesity (24%) and decreased fertility (10%). Excluding these, Group B (HR 5.3, 95% CI 1.6-17.3) and Group C (HR 5.7, 95% CI 1.7-19.0) survivors remained at increased risk of having ≥1 chronic condition. Group A survivors showed a similar HR without statistical significance (HR 4.0, 95% CI 0.5-31.3). Three survivors died during study follow-up (SMR 6.5, 95% CI 1.3-19.0), only one died due to a non-cancer related cause of death. All Groups (A-C) were more likely than siblings to report impaired functional status (OR 11.2, 95% CI 3.5-35.6; 4.5, 95% CI 1.5-13.1; and 15.1, 95% CI 6.0-37.8, respectively). Groups B and C survivors were more likely to report poor mental health (OR 2.9, 95% CI 1.0-8.6 and 3.7, 95% CI 1.0-12.9, respectively), while Group B survivors were more likely to report poor general health (OR 5.1, 95% CI 2.2-11.9). No associations with activity limitations (p's>0.1) or sociodemographic differences (educational level less than a college degree, p's>0.1; household income less than $60,000/year, p's>0.1) were identified in any Groups. Cancer-related pain and anxiety did not differ in Groups B or C compared to survivors in Group A (p=0.9 and 0.2, respectively). Conclusions: Despite excellent survival rates, children diagnosed with B-NHL and treated with contemporary LMB chemotherapy regimens are at risk for chronic health conditions and health status limitations by 14 years from diagnosis. Studies exploring the trajectory of these findings and the impact of early interventions are needed to inform future frontline treatment protocols.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.